Understanding Polyposis Syndromes
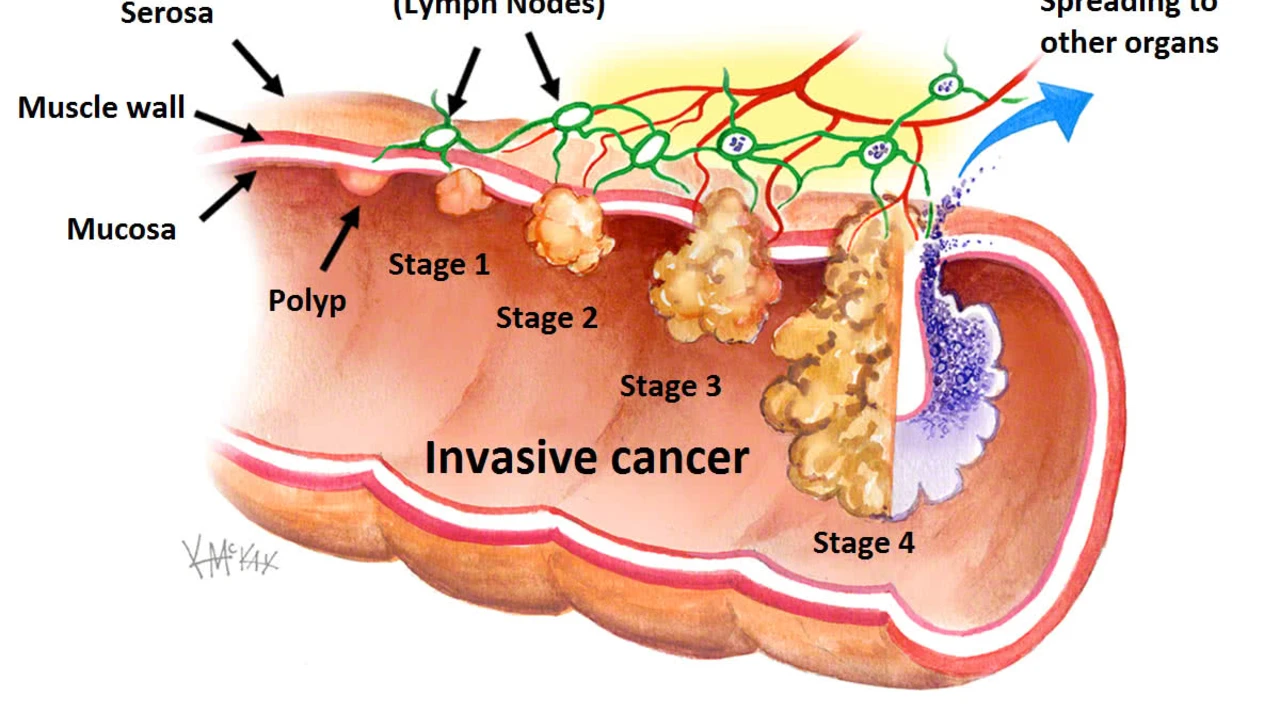
Now, let's dive deep into the nitty-gritty of polyposis syndromes. Imagine this: Your internal garden, the colon, is sprouting little growths, like weeds in a pristine lawn. These aren't just any growths; they're polyps, and in some cases, too many of these cheeky critters are a sign of a polyposis syndrome. Think of it like your garden party guests deciding to bring their friends, and their friends' friends, until the garden's chock-full, and someone's bound to step on your prize roses! Polyposis syndromes such as Familial Adenomatous Polyposis (FAP) show up uninvited, with a genetic RSVP, making your colon their prime real estate. With hundreds, even thousands, of polyps, the colon becomes a bustling metropolis for potential troublemakers that can progress to cancer.
The When and Why of Prophylactic Surgery
Prophylactic surgery, basically a pre-emptive strike in our war against colon cancer, is like sending in the super-nannies of the medical world to sort out the unruly kids before they become outright delinquents. But timing is everything. It's like knowing exactly when to pull those extra-chatty guests away from the mirage of unlimited hors d'oeuvres. If you act too soon, you may rob someone of their natural ability to munch away at life's appetizers. Wait too long, and the party gets out of control. So, when do we gate crash this polyposis party? The decision leans on factors like the type of polyposis syndrome, the number, size, and histological sassiness of these polyp partygoers, and the patient's personal and familial risk factors. It's a complex RSVP list to handle, and it definitely requires finesse.
Types of Prophylactic Surgeries
To tackle these unwanted intruders, a variety of surgical interventions are on the menu. Like choosing dinner at a fancy restaurant, there's more than one tantalizing option. First on the list is a colectomy, a fancy term for evicting the entire colon but leaving the rectum, typified by the phrase 'You don't have to go home, but you can't stay here' to those polyps. But, for those at high risk, such as our FAP friends, a proctocolectomy might be the special of the day. This is like saying, 'The party's over, everybody out!' as it takes the rectum along with the colon. Still, we're left puzzling over what to do with the remnants of the party – rebuilding a functional digestive track is akin to post-party cleanup, involving intricate creativity, a bit of plumbing, and several return trips to the hardware store.
Indications for Prophylactic Surgery in Polyposis
Choosing when to undergo prophylactic surgery is like choosing when to salvage your garden from the weeds. There are clear signals, like finding thousands of polyps, which is akin to seeing your tulips obliterated under a sea of dandelions. Genetic tests, too, play a role in mapping the target area, akin to knowing where your roses are most likely to get trampled. The indications are not always about what's there now but about what could happen if we don't act – it's a prediction game, like knowing it's going to rain on your parade unless you pop up that marquee. High-risk factors include a confirmed diagnosis of a syndrome like FAP or a looming family history that reads like the credits of a horror movie – where you start to suspect everyone may not have made it out alive.
Alternate Treatment Options
We mustn't forget that not everyone is up for a garden overhaul. For those on the fence about prophylactic surgery, there's a buffet of alternative treatments out there. Like choosing a less invasive garden path, endoscopic surveillance brings out the tiny cameras and tools to nip those pesky polyps in the bud. It's less drastic – like deciding to pluck weeds by hand rather than calling in the rototiller. Medications, too, play a part in the game, with celecoxib showing up like a weed preventer, potentially slowing down polyp multiplication. But, as with any treatment, it's not all sunshine and roses; there's always the possibility of side effects, which, like unwanted garden pests, can add complications to your carefully tended beds.
Factors Influencing Decision Making
Choosing to go under the knife is a major decision, one that requires a Torquemada-level of self-interrogation. It's not unlike planning a major event – say a wedding or a milestone birthday bash – where everything from the guest list (family history) to the venue (surgical options) needs meticulous attention. Age, health status, personal preferences, and even the potential for postoperative frolicking (quality of life concerns) waltz into this elaborate decision-making dance. It's not just about ticking boxes on a form; it's about looking at the whole garden and deciding if you're ready for a landscape makeover or if a few tweaks here and there will suffice.
The Procedure and Post-Op Care
Now, strap in for the rollercoaster ride of the actual surgery. Once the decision is made, preparation is key – it’s like gearing up for the biggest, baddest garden party of the year. The procedure itself is a tour de force of medical skill – surgeons become maestros with scalpels, orchestrating the removal of the problematic tissue. After the surgery, it’s all about nurturing your body back to health, akin to coaxing your garden back to life after a harsh winter. Changes in diet, the frequency of follow-up visits, and the adaptation to a new normal are all part of the post-op serenade. And let’s not forget the psychological aspect; it’s a big change, like when Max, my Golden Retriever, realized the backyard was no longer just his domain post-renovation.
Lifestyle Considerations Post-Surgery
Adventure doesn't end with the last stitch. Post-surgery life is like stepping onto a newly terraced garden; it's different, sure, but it has its perks. You might need to adjust your diet, possibly saying fond farewells to some favorite noshes, much like retiring those tacky garden gnomes that don't quite fit your new aesthetic. Physical activity too, will need a rethink – like planning your garden's new footpath, each step forward needs consideration. It's a lifestyle renovation, a chance to rebuild in a way that's sustainable and health-focused, reducing the chance of your garden – or your colon – from falling into disarray once again.
Conclusion: Navigating the Journey Ahead
The journey through prophylactic surgery and polyposis management is like a grand expedition through your own personal wilderness. It requires preparation, bravery, and, crucially, the right team of guides – your medical professionals. Akin to a well-planned safari, it's full of risks and wonders, but the outcome is a reclaimed territory, free from the invasive species of polyps. Making the decision isn't easy, but with information, a sprinkle of humor, and a dash of support, it feels less like facing a lion and more like an encounter with a particularly stubborn bush. As the sun sets on our guide through the wilds of polyposis management, remember that knowledge is power, and in power, there's hope for a polyp-free future.
Kate Taylor
Navigating the decision matrix for prophylactic surgery in polyposis syndromes demands a multidisciplinary approach, integrating genetics, gastroenterology, and surgical oncology. First, the molecular characterization of the APC mutation provides a prognostic index that can stratify patients into high- versus moderate-risk categories. Patients harboring pathogenic truncating variants typically exhibit early polyp burden escalation, warranting surveillance intervals as short as six months. Second, endoscopic phenotyping, including size, histologic dysplasia grade, and morphologic subtype, informs the threshold at which surgical intervention becomes advisable. The literature consistently demonstrates that a cumulative polyp count exceeding 1000 markedly increases the probability of malignant transformation, especially when villous architecture predominates. Consequently, a total proctocolectomy with ileal pouch-anal anastomosis remains the gold-standard definitive therapy for classic FAP presentations. Nevertheless, for attenuated FAP or MUTYH-associated polyposis, segmental colectomy may suffice, provided that diligent postoperative surveillance is maintained. From a perioperative standpoint, minimally invasive laparoscopic techniques have reduced morbidity rates, shortening hospital stays to an average of three to five days. Enhanced recovery after surgery (ERAS) protocols, encompassing multimodal analgesia and early ambulation, further optimize functional outcomes. Postoperatively, nutritional counseling is paramount, as patients must adapt to altered bowel physiology and potential short bowel syndrome risks. Psychosocial support services, including patient advocacy groups, can mitigate the emotional impact of life-altering gastrointestinal reconstruction. Clinicians should also discuss fertility considerations, given that pelvic surgery may influence reproductive anatomy in younger patients. Importantly, shared decision-making models empower patients to weigh quality-of-life trade-offs, such as pouchitis risk versus cancer prophylaxis. Emerging pharmacologic agents, like selective COX-2 inhibitors, are under investigation for chemopreventive adjuncts, though their long-term efficacy remains uncertain. In summary, individualized risk assessment, coupled with evidence-based surgical planning, maximizes oncologic safety while preserving functional independence. I encourage anyone facing these complex choices to seek a second opinion and to engage actively with their care team.
Hannah Mae
i dont think all these surgeries are necessary, you could just live with the polyps.
Iván Cañas
The decision timeline for prophylactic colectomy often hinges on both polyp load and family history, which is why many guidelines set a threshold around age 20 for classic FAP. In practice, we balance the surgical risks against the long‑term benefit of cancer prevention. It's also essential to consider the patient's nutritional status before operating, as malnutrition can impair healing. Multidisciplinary tumor boards can help clarify individual risk factors and personalize the surgical plan. Ultimately, open communication with the patient fosters trust and leads to better adherence to postoperative surveillance.
Jen Basay
I totally get how overwhelming the options can feel 😊.
Having a clear roadmap with regular check‑ups really eases the anxiety.
It’s great that you highlighted the psychosocial support side too.
Hannah M
Your encouragement really shines through 😄.
Remember, patients often find comfort in community forums where shared stories reduce isolation.
A little humor can make the tough recovery journey a bit brighter 🌟.
Poorni Joth
Honestly, suggesting people just ignore a known cancer risk is morally abhorrent.
You cant be serious about letting polyps run wild; it's a death sentence waiting to happen.
The medical community works hard to educate, not to push aggressive surgeries without reason.
Wake up and think about the real consequences.
Yareli Gonzalez
While it's important to emphasize the seriousness, each individual's circumstances deserve careful consideration.
A balanced approach that respects both medical evidence and personal values is key.
Alisa Hayes
I agree, the nuance matters.
Sometimes patients feel pressured, and that can backfire.
Clear, jargon‑free explanations empower them to make informed choices.
Let’s keep the dialogue open.
Mariana L Figueroa
Surgical timing is indeed a balance of risk and benefit.
Using ERAS protocols shortens recovery and improves outcomes.
Keep the patient at the center of every decision.
mausumi priyadarshini
Absolutely, the balance you mention, however, must also include genetic counseling, lifestyle adjustments, and long‑term follow‑up; otherwise the picture remains incomplete.
Moreover, when discussing benefits, we should reference statistical outcomes, patient preferences, and institutional expertise, all of which shape the final recommendation.
Carl Mitchel
From a purely evidence‑based perspective, the data clearly support early colectomy in classic FAP.
Delaying surgery contrary to guideline recommendations is simply reckless.
Patients deserve the best standard of care, not an optional gamble.
Suzette Muller
I understand the urgency you describe, and I’ve seen many patients benefit from timely intervention.
Yet, I’ve also encountered cases where a tailored, less invasive approach improved quality of life.
It’s vital to weigh both the statistical outcomes and the individual’s lived experience.
Josh SEBRING
Sure, guidelines are cool, but they don’t cover every unique case.
Sometimes you have to trust gut instinct over textbook rules.