Autoimmune Liver Disease: Easy Guide & Common-Sense Support
Ever wondered why your immune system might attack your own liver? That’s exactly what happens in autoimmune liver disease. It sounds rare and complicated, but it’s more common than most folks think—and it’s a serious health issue that benefits from real answers, not medical jargon.
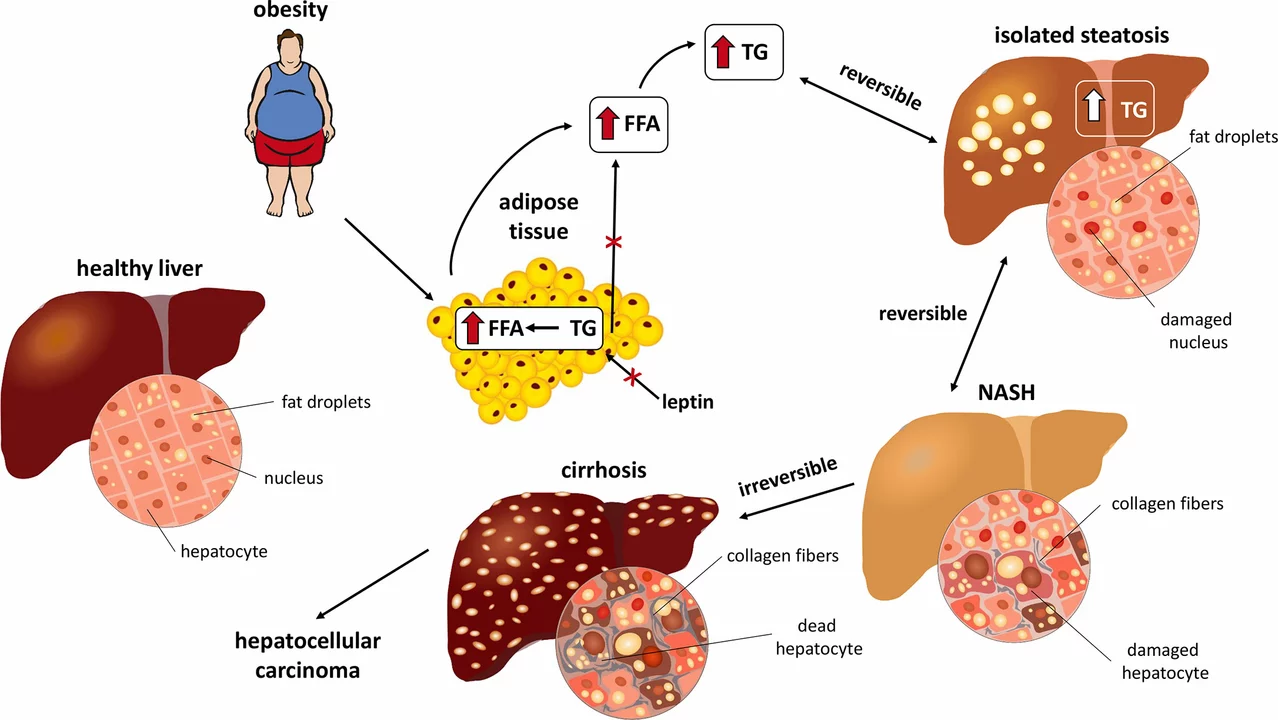
At its heart, autoimmune liver disease is when your body mistakes healthy liver tissue for something dangerous and sends the immune system into attack mode. This creates ongoing inflammation and can damage the liver over time. People sometimes notice symptoms like feeling tired all the time, yellowing of the skin (that’s jaundice), itchy skin, dark pee, or pain in the upper right belly. These signs aren’t unique—so doctors rely on specific blood tests and scans to get a proper diagnosis. If something feels off for more than a few weeks, it’s not just stress or bad luck—seeing a doc makes a difference early on.
There isn’t just one kind of autoimmune liver disease, either. The top ones are autoimmune hepatitis, primary biliary cholangitis (PBC), and primary sclerosing cholangitis (PSC). Each has its quirks. For example, autoimmune hepatitis can show up out of the blue at any age, while PBC most often pops up in women over 40. PSC is tricky too—many who get it also deal with other immune issues like inflammatory bowel disease.
Treatment is practical and aimed at settling down the overactive immune response. Doctors usually start with steroids or immune-suppressing meds, and sometimes introduce newer drugs if those don’t work out. You’ll hear a lot about regular bloodwork and follow-up visits, because these conditions need close watching. The goal? Prevent ongoing liver damage and help you keep living life on your own terms.
Managing autoimmune liver disease isn’t all pills and doctor visits. Everyday choices matter, too. Eating a balanced, liver-friendly diet—think less alcohol, less fat, and more fresh food—makes a real difference. People living with these conditions often talk about how staying active, getting enough sleep, and keeping stress in check help them handle flare-ups and fatigue. Tracking symptoms, keeping a question list for appointments, and building a good relationship with healthcare teams can put you in the driver’s seat.
If you’re facing autoimmune liver disease or supporting someone who is, the best thing you can do is stay informed and ask questions. There are new treatments and research all the time, so there’s real reason for hope. You don’t have to figure it out alone—connecting with liver health groups and hearing from others living with the same diagnosis can be surprisingly helpful. Nobody chooses this road, but you can choose to get answers and support that actually work for you.
The Connection Between Hepatic Encephalopathy and Autoimmune Liver Disease
In my latest research, I've discovered a fascinating connection between hepatic encephalopathy and autoimmune liver disease. Hepatic encephalopathy is a neuropsychiatric disorder that occurs when the liver fails to eliminate toxins from the bloodstream, which in turn affects the brain. Autoimmune liver disease, on the other hand, is when our immune system mistakenly attacks and damages our liver cells. It turns out that autoimmune liver diseases, such as autoimmune hepatitis or primary biliary cholangitis, can lead to liver damage and impair its function. As a result, this can cause a buildup of toxins in the bloodstream, eventually leading to the development of hepatic encephalopathy. It's crucial for us to be aware of these connections to better understand, prevent, and treat such conditions.