When a child breaks out in hives after eating a peanut butter sandwich-or an employee struggles to breathe after a shrimp-laced lunch-the difference between life and death often comes down to one thing: anaphylaxis action plan. It’s not just paperwork. It’s a lifeline. And too many schools and workplaces still treat it like an afterthought.
Anaphylaxis doesn’t wait for office hours or school bell schedules. It strikes fast. In the U.S., about 8% of children have food allergies that can trigger this deadly reaction. For adults, the numbers are rising too. And when it happens, every second counts. Studies show that delaying epinephrine by more than five minutes increases the risk of death by 83%. That’s not a statistic-it’s a warning. This isn’t about being cautious. It’s about being ready.
What Exactly Is an Anaphylaxis Action Plan?
An anaphylaxis action plan is a clear, written guide that tells exactly what to do when someone has a severe allergic reaction. It’s not a vague reminder. It’s a step-by-step emergency script. Every major health organization-from the CDC to FARE (Food Allergy Research & Education)-agrees on the core elements. A good plan includes:
- A photo of the person at risk
- Confirmed allergens (like peanuts, shellfish, or latex)
- Specific symptoms to watch for
- Clear instructions on when and how to use epinephrine
- Emergency contact numbers
- Signature from a licensed doctor
There’s no room for guesswork. Vague language kills. Dr. Ruchi Gupta from Northwestern University says it plainly: "The single most important element is unambiguous epinephrine administration instructions." If the plan says "call 911 first," or "wait to see if it gets worse," it’s already failed.
Why Schools Are Ahead (But Still Falling Short)
Schools have made real progress. Since the CDC released its Voluntary Guidelines in 2013-and updated them in 2020 and 2024-most U.S. school districts now have formal policies. Forty-nine states have laws requiring schools to have epinephrine available. Some even mandate stock epinephrine that doesn’t belong to any one student-so any child in distress can get help immediately.
But here’s the problem: having a plan on paper doesn’t mean it works. A 2022 survey by the National Association of School Nurses found that:
- Only 37% of schools provide annual staff training
- 22% keep epinephrine locked in cabinets
- 41% are still using outdated forms from years ago
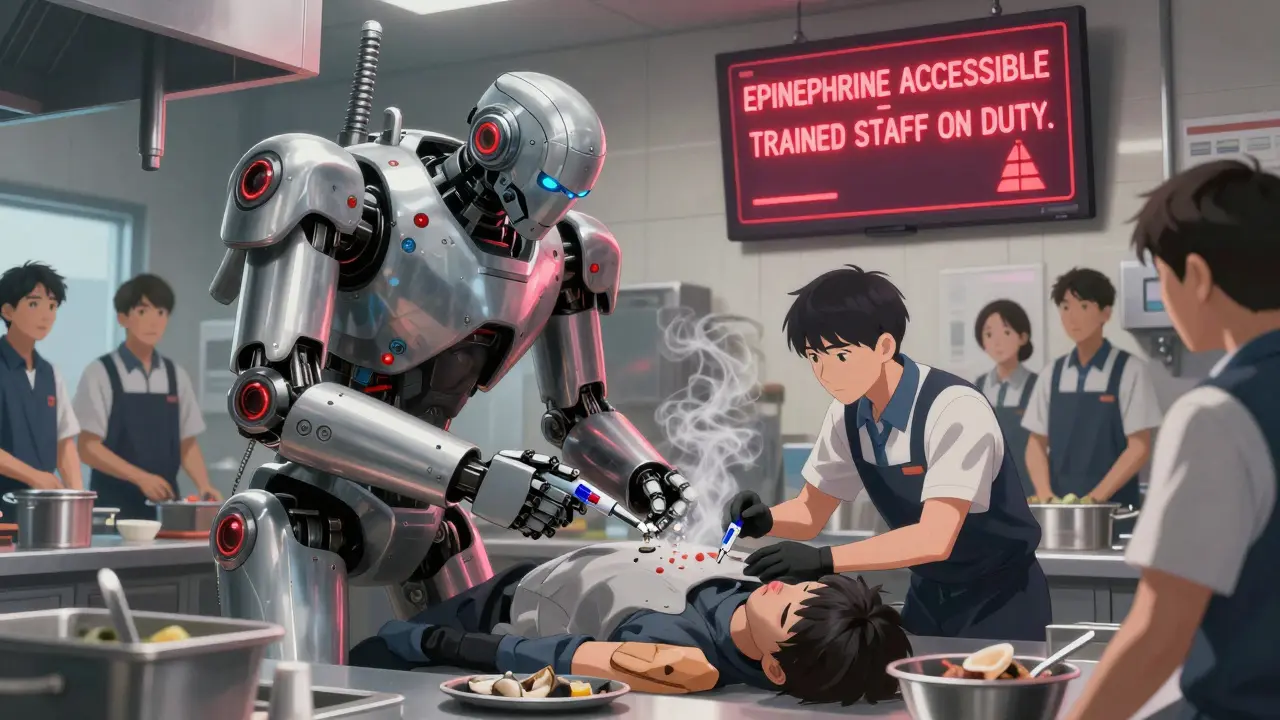
Epinephrine must be unlocked, visible, and within 60 seconds of reach. If it’s tucked away in a nurse’s office and the nurse is at lunch? That’s a death sentence. New York State’s 2024 guidelines say it clearly: "Epinephrine must be stored at room temperature, not in locked cabinets, and accessible within 60 seconds."
Successful schools don’t just hand out forms. They train everyone. At least two staff members per classroom know how to use an EpiPen. Teachers, bus drivers, cafeteria workers, and even playground aides get trained. FARE’s digital action plan platform, launched in March 2024, lets schools update emergency contacts in real time. It’s been adopted by 22% of districts-and those schools report faster responses and fewer complications.
Workplaces? Still in the Dark Ages
While schools have laws, training, and funding, workplaces are stuck in the 1990s. Only 28 states have any formal anaphylaxis policies for employers. The Americans with Disabilities Act says employers must provide reasonable accommodations-but that doesn’t mean they do.
Think about it: a server with a shellfish allergy works in a kitchen. Their epinephrine is locked in a drawer behind the counter. When they start wheezing, they have to sneak away to the bathroom to inject themselves. That’s not a hypothetical. It happened. And it’s not rare.
A FARE survey of 850 employees with severe allergies found that 57% experienced at least one workplace reaction where coworkers hesitated to help. Why? Fear of legal liability. Fear of doing it wrong. Fear of not knowing what to do.
OSHA’s guidelines are vague. They say employers should have first aid supplies-but they don’t specify epinephrine. No one trains staff. No one tests readiness. And with high turnover in retail, hospitality, and food service, even if you train someone this month, they’re gone by next quarter.
There’s no national standard. No funding stream. No mandatory drills. That’s why only 34% of U.S. employers have any formal anaphylaxis protocol at all.
The Critical Components: What Must Be in Every Plan
Whether it’s a school or a workplace, the plan must include these non-negotiables:
- Epinephrine as first treatment-not antihistamines, not waiting, not calling 911 first. Epinephrine goes in the thigh immediately when two or more body systems are affected (like skin + breathing, or skin + stomach).
- Clear symptom checklist-Mild: hives, itching, swelling. Severe: throat closing, wheezing, dizziness, passing out. If you see one severe sign, give epinephrine. Don’t wait for more.
- Two doses available-One might not be enough. A second dose may be needed within 5-15 minutes if symptoms don’t improve.
- Training for everyone-Not just the nurse or HR rep. Bus drivers, cashiers, warehouse workers, janitors-all of them need to know how to use an auto-injector. The American Academy of Pediatrics now says universal training is essential.
- Annual review-Allergies change. Medications expire. Contacts update. Plans older than a year are dangerous.
FARE’s 2023 template scored 4.7 out of 5 from educators. Generic school forms? Only 2.8. The difference? Clarity. Simplicity. No jargon. No legalese. Just: "If this happens, do this. Now."
Real Stories: Success and Failure
One mother, Sarah Johnson, shared how her daughter’s school used FARE’s plan with video training. When her daughter accidentally ate a peanut-contaminated snack, the teacher recognized the symptoms-hives and coughing-gave epinephrine in 90 seconds, and called 911. No hospital stay. No long-term damage. Just a quick, calm response.
Compare that to the Reddit post from a server who had to inject herself in the bathroom because her manager refused to unlock the epinephrine. "It’s against policy," he said. That’s not policy. That’s negligence.
The data backs this up. Schools using standardized plans had a 65% success rate in emergency responses. Those using generic forms? Only 28%. In workplaces? The failure rate is even higher. Fear, ignorance, and lack of structure cost lives.
How to Fix This-Now
If you’re a school administrator: Adopt FARE’s or CDC’s official template. Train at least two staff per classroom. Store epinephrine in a bright, unlocked, wall-mounted case. Update plans every year. Hold drills. Make it routine.
If you’re an employer: Start with one simple rule: "If someone has a known severe allergy, their epinephrine must be accessible within 60 seconds, no exceptions." Train new hires during orientation. Add allergy response to your safety manual. Don’t wait for someone to die before you act.
If you’re a parent or employee with allergies: Demand a written plan. Don’t accept a verbal promise. Ask for a copy. Verify it’s signed by a doctor. Check that epinephrine is stored properly. Push for training. Be the one who refuses to let it slide.
What’s Next?
The future is here. FARE’s digital plan platform lets schools update contacts instantly. The FDA is testing voice-guided epinephrine injectors for 2025-devices that will talk you through the steps, even if you’ve never used one before. That’s the kind of innovation workplaces need.
Dr. Robert Wood from Johns Hopkins calls anaphylaxis plans "essential infrastructure," like AEDs for heart attacks. We don’t ask if a gym should have a defibrillator. We assume it does. The same should be true for epinephrine in schools and workplaces.
This isn’t about being perfect. It’s about being prepared. One plan. Two doses. One trained person. That’s all it takes to save a life. And if you’re not doing it-you’re risking someone’s.
What are the signs of anaphylaxis?
Anaphylaxis affects at least two body systems. Mild symptoms include hives, itching, swelling of lips or face, runny nose, or mild nausea. Severe symptoms that require immediate epinephrine include difficulty breathing, throat tightness, wheezing, dizziness, rapid pulse, vomiting, or loss of consciousness. If you see even one severe symptom, give epinephrine right away-don’t wait for more.
Why is epinephrine the only treatment?
Epinephrine is the only medication that stops the body’s dangerous overreaction during anaphylaxis. Antihistamines (like Benadryl) can help with mild itching or hives, but they do nothing for airway swelling, low blood pressure, or shock. Delaying epinephrine to give antihistamines first increases the risk of death. Epinephrine saves lives. Everything else comes after.
Can anyone use an EpiPen?
Yes. EpiPens are designed for non-medical people to use. They’re simple: remove the cap, jab against the outer thigh, hold for 3 seconds. Training takes 15 minutes. Most people can do it after one demo. Schools and workplaces that train everyone-even janitors and bus drivers-see faster responses and fewer deaths.
What if I’m scared to give epinephrine?
Fear kills more than allergies. The CDC and FARE both say: "When in doubt, give it." Epinephrine is safe. Giving it when it’s not needed may cause a racing heart or shaking-but it won’t harm someone who’s not having anaphylaxis. Not giving it when they are? That’s fatal. Training reduces fear. Practice reduces panic. Make it routine.
Do I need a doctor’s note for an anaphylaxis action plan?
Yes. A valid plan must be signed by a licensed physician or nurse practitioner. It should list confirmed allergens, symptoms, and epinephrine instructions. A handwritten note or verbal permission is not enough. Schools and employers are legally protected when they follow a signed medical plan. Without it, they’re flying blind.
How often should an anaphylaxis plan be updated?
Every year. Allergies can change. Medications expire. Emergency contacts move. The CDC recommends annual reviews, and New York State’s 2024 guidelines require it. Outdated plans are dangerous. If the plan hasn’t been reviewed in over a year, it’s not reliable. Treat it like a fire drill-check it, test it, update it.
Are schools required to have stock epinephrine?
In 38 U.S. states, yes. Stock epinephrine is not assigned to one student-it’s kept on hand for any person in need. The CDC encourages this. Schools with stock epinephrine have responded to 17% more anaphylaxis events than those without it. Even if a student doesn’t have a known allergy, someone else might have a reaction. Stock epinephrine saves lives.
What should a workplace do if an employee has a severe allergy?
Under the ADA, employers must provide reasonable accommodations. That means: keeping the employee’s epinephrine accessible, training coworkers on how to use it, removing known allergens from common areas, and updating emergency procedures. It’s not optional. A 2022 FARE survey found 57% of workers with allergies had a reaction where colleagues didn’t help. That’s not just dangerous-it’s illegal.

Daniel Dover
Epinephrine should be as accessible as a fire extinguisher. Period. If your school or workplace can’t guarantee that within 60 seconds, they’re not just negligent-they’re dangerous.
Charlotte Dacre
Oh wow, a workplace actually has to *do* something for once? Shocking. I guess next they’ll start requiring oxygen tanks in elevators too.
Chiruvella Pardha Krishna
Human life is a fragile thread woven by circumstance, not policy. The anaphylaxis plan is not a solution-it is a symptom of a society that refuses to confront mortality directly. We institutionalize fear because we are too afraid to live without it.
Yet, in the silence between breaths, when the EpiPen is locked away, we forget: death does not negotiate. It does not wait for forms. It does not care if the nurse is at lunch.
The tragedy is not that we lack plans-it is that we mistake paperwork for preparedness. A signature on paper does not save a life. A hand that moves does.
We are not failing because we are ignorant. We are failing because we are comfortable with the illusion of control.
And so we bury our responsibility in bureaucratic language-"reasonable accommodations," "guidelines," "recommended practices."
But when the throat closes, there are no guidelines. Only the trembling hand. Only the moment. Only the choice.
Will you act? Or will you wait for someone else to do it?
Mandeep Singh
Let me tell you something-this whole conversation is laughable. You think a piece of paper with a doctor’s signature saves lives? No. Training does. Consistency does. Accountability does. And yet here we are, in 2025, still treating this like a checklist item instead of a survival imperative.
My cousin works in a school district where they have a 100% compliance rate-epinephrine on every floor, unlocked, labeled, and drilled into staff every month. Guess what? They’ve had zero deaths since 2019. Zero. Not one.
Meanwhile, your "workplace" probably has a dusty box in HR labeled "emergency supplies" that no one’s opened since 2017. And you wonder why people die? It’s not because the science is unclear. It’s because the culture is lazy.
Stop romanticizing paperwork. Start demanding action. If your manager says "we don’t have the budget," ask them how much a funeral costs. Ask them how much a lawsuit costs. Ask them how much guilt costs.
And if they still don’t move? Quit. Find a place that values life more than liability.
Kaye Alcaraz
Every school and workplace should have two trained staff members per building with epinephrine within arm's reach at all times. No exceptions. No excuses. No "we'll get to it next quarter."
It's not expensive. It's not complicated. It's not optional. It's basic human decency.
Train everyone. Store it visibly. Update it annually. Test it like a fire drill. That's it. That's all we need.
And if you're reading this and you're not doing this? You're not just behind. You're endangering people.
Sarah Barrett
There’s something quietly horrifying about how we’ve normalized the idea that someone’s life hinges on whether a janitor remembers where the EpiPen is-or if the nurse took her lunch break.
We treat anaphylaxis like a glitch in the system, not a guaranteed eventuality. But it’s not a glitch. It’s biology. It’s physics. It’s time. And time doesn’t care about your policy manual.
The real tragedy isn’t the lack of epinephrine. It’s the lack of urgency. We’ll install ADA ramps, but we won’t unchain a life-saving device because "it’s not in the budget."
It’s not just negligence. It’s a moral failure dressed in HR jargon.
Erica Banatao Darilag
i just want to say that i had a friend who had a reaction at work and no one knew what to do. they called 911 first and waited 8 minutes. she almost died. the epipen was in a drawer. the manager said he was scared to use it. i cry every time i think about it.
please. just train people. it takes 15 minutes. it could save someone you know.
Kapil Verma
India has been doing this right for decades. In rural clinics, we don’t wait for paperwork. We act. We train the village nurse, the schoolteacher, the auto driver. We don’t need a 20-page form. We need courage.
Why does America need a federal mandate to save a life? Because you’ve turned compassion into bureaucracy. Because you’ve confused compliance with care.
Your system is broken. Ours isn’t perfect-but we don’t wait for permission to save someone. We just do it.
Michael Page
Is it possible that the real issue isn’t epinephrine access, but the medicalization of everyday life? We’ve turned allergies into existential emergencies because we’ve lost the ability to tolerate uncertainty.
What if we focused less on emergency protocols and more on building resilience? On reducing environmental triggers? On rethinking food systems?
Or are we too comfortable with the illusion of control-believing that if we just have the right tool, we’ve solved the problem?
Perhaps the deeper question isn’t where the EpiPen is stored-but why we’ve allowed our society to become so fragile.
Joe Grushkin
Oh look, another woke manifesto disguised as public health advice. Next they’ll mandate oxygen masks for people who sneeze too hard.
Let me guess-you think every workplace needs a full-time allergist on standby? Maybe we should just stop having food at work entirely. Or ban peanut butter. Or make everyone carry a medical ID.
Here’s a radical idea: let people with allergies manage their own risk. Don’t force me to train my barista to inject my friend with a needle because you’re too scared to read a label.
Personal responsibility isn’t dead. It’s just inconvenient for you.
Betty Kirby
Let me be crystal clear: if your workplace or school doesn’t have a working epinephrine protocol, you’re not just unprepared-you’re a liability. And anyone who says "we don’t have the budget" is either lying or morally bankrupt.
I’ve seen the aftermath. I’ve held the hand of a teenager who didn’t make it because someone thought "maybe it’ll pass."
There is no nuance here. No gray area. No "but we’re busy."
Epinephrine is not a luxury. It’s not a suggestion. It’s not a compliance checkbox.
It’s the difference between a funeral and a birthday party.
And if you’re still hesitating? You’re not just failing the system. You’re failing the people who trust you to keep them alive.