Imagine getting sick every few weeks - sinus infections, pneumonia, stomach bugs - and no matter how many antibiotics you take, you just can’t shake it off. For people with Common Variable Immunodeficiency (CVID), this isn’t rare. It’s everyday life. CVID is one of the most common serious immune disorders you’ve never heard of. It’s not allergies. It’s not asthma. It’s a broken system inside your body that can’t make the antibodies needed to fight off germs. And without those antibodies, even a common cold can turn dangerous.
What Exactly Is CVID?
CVID stands for Common Variable Immunodeficiency. It’s a genetic disorder where your B cells - the part of your immune system that makes antibodies - don’t work right. You might have plenty of B cells, but they’re stuck. They can’t mature into the kind that produce IgG, IgA, and sometimes IgM antibodies. These are the proteins that act like soldiers, tagging bacteria and viruses so your body can destroy them. When those levels drop too low, your body becomes defenseless.
Doctors diagnose CVID when blood tests show IgG levels below 500 mg/dL (normal is 700-1600), IgA below 7 mg/dL (normal is 70-400), and poor response to vaccines like pneumococcus or tetanus. It’s not something you’re born with and immediately notice. Most people don’t start showing symptoms until their 20s or 30s. That’s why it often takes years to get diagnosed - an average of 8 years, according to patient surveys. Many see three or more doctors before someone finally runs the right tests.
Why Antibody Deficiency Matters
Antibodies aren’t just for colds. They protect you from serious infections. In CVID, the most common problems are respiratory. About 35% of pneumonia cases in CVID patients are caused by Haemophilus influenzae, 28% by Streptococcus pneumoniae, and 15% by Staphylococcus aureus. These aren’t rare bugs - they’re common ones that healthy people shrug off. But for someone with CVID, they stick around, cause damage, and can lead to permanent lung scarring. By age 50, 65% of untreated CVID patients develop chronic lung disease. That’s more than four times the rate in healthy adults.
It’s not just the lungs. About half of CVID patients deal with gut issues. Chronic diarrhea, weight loss, bloating - these aren’t just "bad digestion." They’re often caused by Giardia lamblia, a parasite that normally affects less than 1% of the population but shows up in 12% of CVID cases. The immune system can’t clear it, so it hangs on, stealing nutrients and causing inflammation.
And then there’s the hidden threat: autoimmunity. About 25% of CVID patients develop autoimmune disorders - their own immune system turns on their body. Immune thrombocytopenia (ITP), where platelets are destroyed, affects 15%. Autoimmune hemolytic anemia (AIHA), where red blood cells are attacked, hits 10%. Some even get rheumatoid-like arthritis. These complications are rare in other antibody deficiencies, making CVID uniquely complex.
How CVID Differs From Other Immune Disorders
It’s easy to confuse CVID with other immune problems. But here’s how it stacks up:
- Selective IgA Deficiency: The most common primary immunodeficiency. Only IgA is low. IgG and IgM are normal. Most people don’t even know they have it - they live normal lives. CVID is far more serious.
- X-linked Agammaglobulinemia (XLA): Affects mostly boys. B cells are nearly gone from birth. Symptoms start in infancy. CVID patients usually have normal B cell counts - it’s the function that’s broken.
- Severe Combined Immunodeficiency (SCID): "Bubble boy" disease. No T cells or B cells. Fatal without a bone marrow transplant. CVID patients have functional T cells - just no antibodies.
CVID sits in the middle - not as immediately life-threatening as SCID, but far more complex than IgA deficiency. It’s not one disease. It’s a group of disorders with similar symptoms but different causes. That’s why finding a single gene mutation has been so hard. Only 15-20% of cases have a known genetic link. Mutations in genes like TACI, BAFF-R, or CD19 show up in some, but not all. For most, the cause remains a mystery.
Immunoglobulin Replacement: The Lifeline
There’s no cure for CVID. But there’s a treatment that changes everything: immunoglobulin replacement therapy. It’s exactly what it sounds like - you get antibodies from healthy donors. These are purified from thousands of liters of human plasma and given as infusions.
There are two main ways:
- Intravenous Immunoglobulin (IVIG): Given every 3-4 weeks through a vein in a clinic or hospital. Dose: 400-600 mg per kg of body weight.
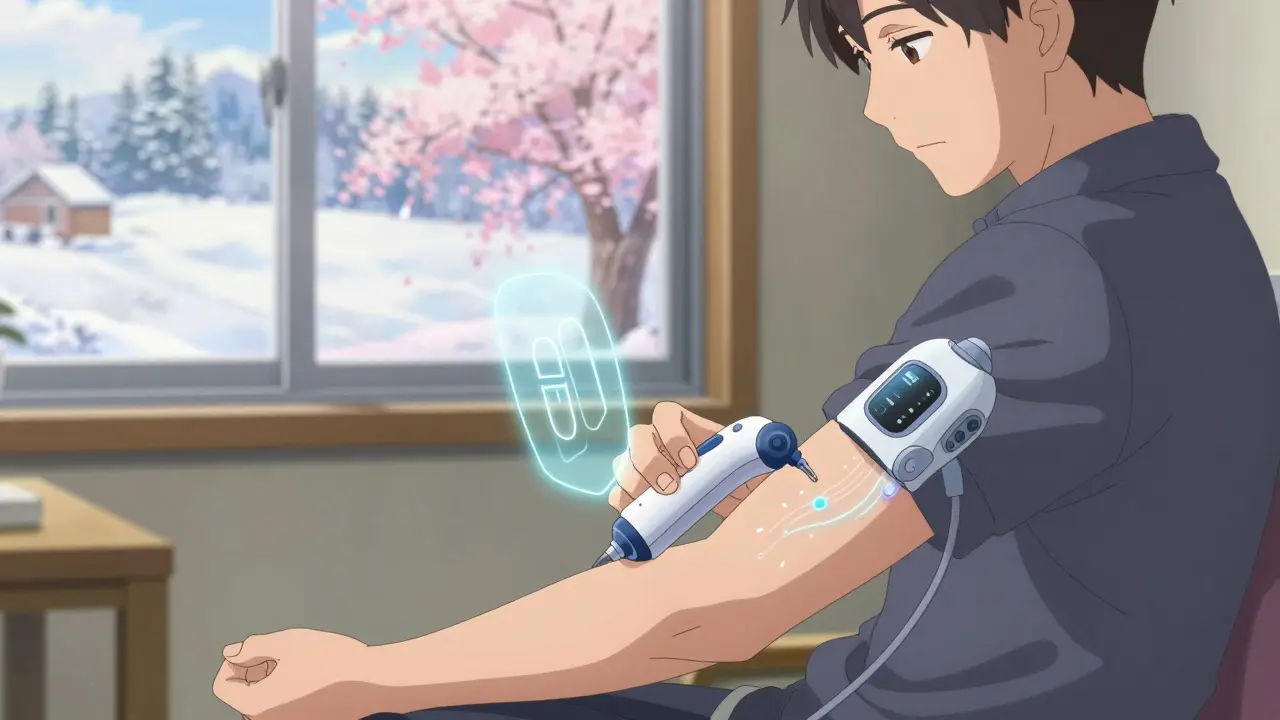
- Subcutaneous Immunoglobulin (SCIG): Injected under the skin, usually weekly. Dose: 100-150 mg per kg. Many patients do this at home after training.
Patients on consistent therapy see dramatic improvements. One 2023 survey found that infection frequency dropped from over 10 per year to just 2.1. Energy levels improved for 78% within three months. Quality of life isn’t just better - it’s restored.
But it’s not perfect. About 32% of IVIG users get side effects: headaches (68%), chills (42%), nausea (37%). SCIG has fewer systemic reactions but can cause local swelling or redness at the injection site - about 25-40% of users. The trick? Rotate sites, use smaller doses more often, and go slow. Most people master home SCIG within 8 weeks with proper training.
The Cost and the Challenge
Immunoglobulin therapy isn’t cheap. In the U.S., IVIG costs $65,000-$95,000 a year. SCIG runs $70,000-$100,000. Globally, only 88% of diagnosed patients in wealthy countries get it. In low-income nations, that number drops to 35%. The World Health Organization calls this a crisis. Plasma supply is shrinking. Demand is rising. Experts predict costs could jump 15-20% annually through 2028.
And yet, without it, life expectancy for CVID patients was only 33 years in the 1970s. Now, with consistent therapy, median survival has jumped to 59 years. That’s not just a number - it’s decades of life regained.
What’s Next? New Treatments on the Horizon
Researchers are working on smarter therapies. One promising drug, atacicept, blocks two proteins (BAFF and APRIL) that mess with B cell function. In Phase III trials, it cut severe infections by 37% compared to standard Ig therapy alone. It’s not a replacement yet - but it could become a powerful add-on.
Genetic testing is also getting better. Experts believe CVID isn’t one disease but five or six distinct subtypes. Within five years, doctors may be able to match patients to targeted treatments based on their specific genetic profile - not just blanket antibody infusions.
For now, the best defense is early diagnosis and consistent treatment. If you’ve had frequent infections since your 20s, if antibiotics don’t seem to help, if you’re constantly tired and losing weight - ask for an immunoglobulin panel. It’s a simple blood test. It could change everything.
Living With CVID: Support and Reality
People with CVID aren’t just patients - they’re survivors. The Immune Deficiency Foundation runs over 200 local support groups and hosts an annual conference with 2,500+ attendees. These aren’t just meetings - they’re lifelines. Patients share tips on managing side effects, navigating insurance, finding experienced doctors, and dealing with the emotional toll.
One woman in Melbourne told her story: "I used to cancel plans every month because I felt like I was dying. Now, after starting SCIG at home, I’m hiking, traveling, even planning a wedding. It’s not a cure. But it’s enough to live."
There’s no shame in needing help. CVID isn’t your fault. It’s not caused by lifestyle, diet, or stress. It’s biology. And science has given us tools to fight back.
Is CVID the same as having low immunity from stress or poor diet?
No. CVID is a genetic disorder where your body can’t make antibodies, no matter how healthy you eat or how much sleep you get. Stress or lifestyle can weaken your immune system temporarily, but they don’t cause the deep, persistent antibody deficiency seen in CVID. Blood tests show specific low levels of IgG, IgA, and poor vaccine response - things that don’t fix with vitamins or rest.
Can you outgrow CVID?
No. CVID is a lifelong condition. The immune system’s defect doesn’t correct itself. While symptoms can improve with treatment, the underlying problem remains. Stopping immunoglobulin therapy leads to a return of infections and complications. Lifelong management is necessary.
Are there side effects from long-term immunoglobulin therapy?
Most people tolerate it well, but long-term use can cause kidney stress, especially with IVIG. Dehydration increases this risk, so staying hydrated is critical. Some patients develop antibodies against the infused immunoglobulins, reducing effectiveness over time. Regular monitoring of kidney function and IgG levels helps manage these risks. SCIG has fewer systemic side effects and is often preferred for long-term use.
Can CVID lead to cancer?
Yes. People with CVID have a 20 to 50 times higher risk of developing lymphoma compared to the general population. Chronic inflammation from recurring infections and autoimmune activity likely contributes. Regular screenings - including abdominal ultrasounds and blood tests - are part of standard care. Early detection saves lives.
How do I know if I have CVID and not just frequent colds?
If you’ve had four or more ear or sinus infections in a year, two or more pneumonias in a year, or chronic diarrhea with weight loss, and antibiotics don’t fully fix it, see an immunologist. A simple blood test measuring IgG, IgA, and IgM levels - plus checking how you respond to vaccines like Pneumovax - can confirm or rule out CVID. Don’t wait for hospitalization. Early diagnosis prevents permanent damage.

Jay Ara
man i had no idea this was so common. my cousin went undiagnosed for 7 years and they thought she was just weak. now she does scig at home and actually goes out again. life changing
Michael Bond
early diagnosis saves lungs. period.
Kuldipsinh Rathod
my uncle had this. he used to get pneumonia every winter. after ivig, he started gardening again. i never thought a blood infusion could do that
SHAKTI BHARDWAJ
so its just rich people who get to live? why is this so expensive when its just donated blood? capitalism is a disease
Matthew Ingersoll
in india, we have plasma donation drives in rural areas. the real crisis isn’t just cost-it’s access. people die because they’re 200km from a clinic, not because they can’t afford it.
carissa projo
there’s something profoundly human about this-how medicine can turn a life from constant hospital visits to hiking trails and wedding plans. it’s not magic. it’s science, yes-but also the quiet, relentless care of nurses, families, and patients who refuse to let a broken immune system define them. this isn’t just treatment. it’s dignity restored.
josue robert figueroa salazar
you think this is bad wait till you get kidney damage from ivig. then you’re just trading one hell for another
Sarah Holmes
How dare you reduce a complex, genetically rooted immunological disorder to a mere financial inconvenience? Your reductionist, emotionally manipulative rhetoric trivializes the lived reality of patients who endure chronic infections, lung scarring, and autoimmune complications-not because of capitalism’s failures, but because of biological unpredictability. This is not a political issue. It is a medical emergency that demands scientific investment, not performative outrage. If you truly cared, you’d advocate for plasma donation expansion, not performative rage.