Switching from brand-name immunosuppressants to generic versions of cyclosporine and tacrolimus can save thousands of dollars a year. But for transplant patients, that savings comes with a hidden risk: tiny differences in how the body absorbs these drugs can trigger rejection, toxicity, or hospitalization.
Why These Drugs Are Different
Cyclosporine and tacrolimus aren’t just any pills. They’re narrow therapeutic index (NTI) drugs, meaning the difference between a safe dose and a dangerous one is razor-thin. For tacrolimus, the target blood level is between 5 and 15 ng/mL. Go below 5, and your body might start attacking the new organ. Go above 15, and you risk kidney damage, tremors, or even seizures.
Both drugs work the same way - they block calcineurin, a protein that turns on immune cells. But that’s where the similarity ends. Tacrolimus is 20 to 100 times more potent than cyclosporine. A typical daily dose of tacrolimus is 5 mg twice a day. Cyclosporine? Around 150 mg twice a day. That’s a 30-fold difference in pill size, yet both are meant to do the same job: keep your immune system from rejecting your new kidney, liver, or heart.
Even more complex: they’re metabolized by the same liver enzyme (CYP3A4), so anything that affects that enzyme - grapefruit juice, antibiotics, antifungals - can throw off your levels. But the real problem isn’t drug interactions. It’s the generics.
The Generic Switch Problem
By 2023, over 92% of tacrolimus and cyclosporine prescriptions in the U.S. were generic. Insurance companies push them hard because brand-name Prograf costs $1,200-$1,500 a month. Generic tacrolimus? $300-$500. Neoral (brand cyclosporine) runs $800-$1,000. Generic cyclosporine? $150-$300.
But here’s the catch: the FDA allows generic versions to vary by up to 25% in how much drug gets into your bloodstream. That’s fine for blood pressure pills. It’s not fine for tacrolimus.
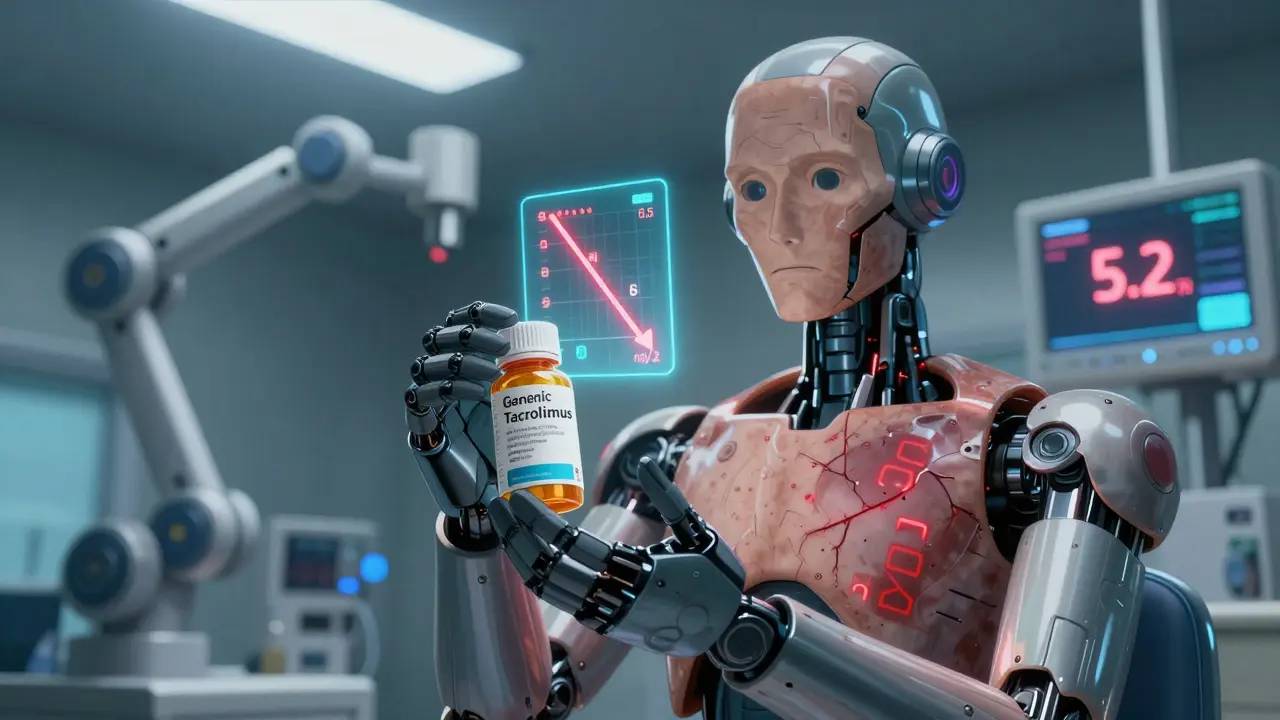
One patient in Sydney switched from brand Prograf to a generic made by Teva. Her blood levels dropped from 8.5 ng/mL to 5.2 in two weeks. She developed mild rejection. She ended up in the hospital. Another patient in Melbourne switched from one generic to another - same drug, different manufacturer - and his levels spiked from 9.1 to 16.7. He got tremors so bad he couldn’t hold a spoon.
These aren’t rare cases. A 2022 survey of 1,247 transplant patients found 42.7% noticed side effects after switching to generic tacrolimus. Nearly 1 in 5 needed a dose adjustment. In the U.S. Renal Data System, non-adherence rates were 15.3% higher among patients on generics - not because they forgot pills, but because they felt something was off and stopped taking them.
Why Generic Versions Aren’t Interchangeable
Not all generics are created equal. Cyclosporine comes in two forms: the old oil-based version (Sandimmune) and the newer microemulsion (Neoral). Even within microemulsion, different manufacturers use different oils, surfactants, and particle sizes. That changes how fast the drug dissolves in your gut.
Tacrolimus is even trickier. The original Prograf is a capsule with a specific coating. Generic versions use different binders, fillers, and capsule shells. One study found that switching between two FDA-approved generic tacrolimus brands caused blood levels to fluctuate by up to 30% - enough to push someone from safe to toxic.
The European Medicines Agency and the FDA both warn: switching between different generic brands without monitoring can lead to rejection or toxicity. The American College of Clinical Pharmacy recommends checking blood levels weekly for the first month after any switch. Most transplant centers now have protocols in place - but not all.

Real Stories, Real Consequences
Reddit’s r/transplant community has over 140 threads since 2023 about generic issues. One user wrote: “My insurance forced me to switch to generic tacrolimus. My levels dropped. I had a biopsy that showed acute rejection. I had to go back on brand - and my insurance refused to cover it.”
Another said: “I’ve been on the same generic for three years. Stable. No problems. Saved me $900 a month.”
That’s the problem. Some people do fine. Others don’t. There’s no way to predict who will react. It’s not about the quality of the generic. It’s about how your body absorbs it - and that’s unique to you.
What You Can Do
If you’re on cyclosporine or tacrolimus, here’s what matters:
- Stick with one generic brand. Once you find one that works, ask your pharmacist to keep giving you the same one. Don’t let them switch you without telling you.
- Get your blood levels checked after every switch. Even if your doctor says it’s “just a generic,” get a level drawn one week after the switch, then again at two and four weeks.
- Know your numbers. Write down your target range. For tacrolimus, it’s usually 5-15 ng/mL. For cyclosporine microemulsion, it’s 100-200 ng/mL (depending on time since transplant). Ask your transplant team what yours should be.
- Avoid grapefruit, pomegranate, and St. John’s wort. These mess with how your body breaks down these drugs.
- Take your pills at the same time every day. Within one hour. Even small changes in timing can affect absorption.
The Bigger Picture
Transplant centers are starting to fight back. By 2023, 67% of major U.S. transplant programs signed contracts with pharmacies to use only one generic manufacturer. That way, patients don’t get switched randomly.
New formulations are coming. In late 2023, Astellas got FDA approval for an extended-release tacrolimus that smooths out blood level spikes. It’s not generic yet - but when it is, it might solve half the problem.
Meanwhile, doctors are starting to use genetic testing. About 20% of people have a gene variant (CYP3A5) that breaks down tacrolimus faster. If you’re one of them, you need a higher dose. Testing for this before starting treatment cuts the time to reach stable levels by 63%.
But none of this matters if you don’t speak up. Insurance companies don’t care about your blood levels. They care about cost. Your pharmacist might not know the difference between generic brands. Your doctor might assume all generics are the same.
You’re the only one who knows how you feel. If your hands shake more, your creatinine climbs, or you feel unusually tired after a switch - tell someone. Demand a blood test. Don’t wait for a rejection episode to prove you were right.
What’s Next
The global market for these drugs is $18.7 billion. Generics make up over 90% of sales. That’s not going to change. But the way we handle them must.
Regulators are finally catching up. In early 2024, the EMA said generic tacrolimus makers must now prove their products work in transplant patients - not just healthy volunteers. That’s a big step.
But until then, the burden falls on you. Know your drug. Know your numbers. Don’t let a $900 monthly savings cost you your transplant.
Can I safely switch between different generic brands of tacrolimus?
No, not without close monitoring. Even though all generic tacrolimus meets FDA bioequivalence standards, switching between different manufacturers can cause blood levels to swing by 20-30%. This can lead to rejection or toxicity. Always check your levels one week after switching and again at two and four weeks. Never switch without telling your transplant team.
Why is tacrolimus more risky than cyclosporine when switching generics?
Tacrolimus has a narrower therapeutic window - its safe range is only 5-15 ng/mL. Cyclosporine’s range is wider (100-200 ng/mL), so small absorption changes are less likely to push you out of range. Also, tacrolimus is absorbed more inconsistently across different generic formulations due to differences in capsule coatings and fillers. Even a 10% change in absorption can push tacrolimus levels from safe to toxic.
How often should I get my blood levels checked after switching to a generic?
Check your levels one week after switching, then again at two and four weeks. After that, continue monthly for the first three months. If your levels stay stable, your doctor may extend the interval. But if you feel off - tremors, nausea, fatigue, or swelling - get tested immediately. Don’t wait for your next scheduled appointment.
Are generic cyclosporine and tacrolimus equally safe?
No. Tacrolimus generics carry higher risk due to their narrow therapeutic index and greater variability in absorption. Cyclosporine generics are more stable, especially the microemulsion version. But both can cause problems if you switch manufacturers without monitoring. The key is consistency - once you find a generic that works, stick with it.
Can I ask my insurance to cover the brand-name drug?
Yes. If you’ve had instability, rejection, or side effects after switching to a generic, your doctor can file a prior authorization request for the brand-name drug. Many insurers approve this if you have documented evidence - like lab results showing level fluctuations - and a letter from your transplant team explaining the risk. Don’t assume it’s denied; fight for it if your health is at stake.
Is there a genetic test that can help with dosing?
Yes. The CYP3A5 gene determines how fast your body breaks down tacrolimus. About 20% of people are “extensive metabolizers” and need higher doses. Testing before starting treatment can reduce the time to reach stable levels by 63%. Ask your transplant pharmacist if this test is available - it’s becoming standard in major centers.
Neil Ellis
Man, I switched to generic tacrolimus last year and didn’t think twice. Turned out my levels dropped like a rock - felt like I was dragging cement shoes every day. Got lucky my doc caught it before rejection kicked in. Now I’m locked in with the same generic brand, and I won’t let them swap it. Save money? Sure. But not at the cost of your new organ.
Lauren Wall
If your insurance forces a switch, fight it. Period.
Tatiana Bandurina
Let’s be real - the FDA’s 25% bioequivalence allowance is a joke for NTI drugs. They test generics on healthy volunteers, not people with zero immune reserve. It’s not about cost. It’s about cutting corners on human life and pretending it’s science. This isn’t a drug policy issue - it’s a systemic betrayal.
Philip House
Look, the U.S. leads the world in transplant success because we don’t let bureaucrats dictate medicine. Generic manufacturers are just trying to make a buck. The real problem? People think ‘FDA-approved’ means ‘safe for everyone.’ It doesn’t. It means ‘meets minimum legal thresholds.’ Big difference.
Ryan Riesterer
Pharmacokinetic variability in tacrolimus generics is well-documented in CYP3A4 polymorphism studies. The coefficient of variation in AUC and Cmax between formulations often exceeds 30%, which is clinically significant in transplant recipients. Monitoring trough levels post-switch is non-negotiable.
Akriti Jain
Big Pharma and the FDA are in bed together. You think this is about safety? Nah. It’s about control. They want you dependent on their system. One brand? One pharmacy? One doctor? That’s not healthcare - that’s a monopoly. And they’re using your transplant to make billions. 🤡💉
Mike P
My cousin got a liver transplant in ’19. Switched to generic cyclosporine - no issues. Saved $1k/month. He’s fine. Meanwhile, you guys act like every single person is gonna die if they get a different pill. Not everyone’s a snowflake. Some of us just want to live without bankruptcy.
shivani acharya
Okay so let me get this straight - the same company makes two different generics of the same drug, and the FDA says it’s fine to swap them like trading baseball cards? But if I switch my coffee brand, I get a stomachache? What’s the difference? Oh right - one’s a life-saving drug and the other’s just a bean brew. So why does the system treat them the same? Because it’s rigged. They don’t care if you live or die - they care if the spreadsheet balances. I’ve been on the same generic for five years. Stable. But I still check my levels every month. Because I don’t trust the system. And I shouldn’t have to.
Brenda King
Just wanted to say thank you for writing this. I’m a transplant nurse and I see this every week - patients scared, confused, and pressured to switch. I always tell them: your body is your ally. If something feels off, it probably is. Keep your levels logged. Know your numbers. And never let a pharmacist make a decision that could cost you your transplant. You’re not being difficult - you’re being smart.
Alec Amiri
Some people are just drama magnets. If you’re stable on generic, don’t panic. Stop making this a crisis. You’re not special. Your body isn’t a magic snowflake. Just take the pill and move on.
Lana Kabulova
Wait - so if I switch from Generic A to Generic B, and my levels spike, is that my fault? Or the manufacturer’s? Or the FDA’s? Or my doctor’s for not warning me? Who’s responsible here? Because if I end up back in the hospital because someone thought ‘close enough’ was good enough - I’m suing everyone.
Rob Sims
Oh please. You think this is new? Back in the 90s, we were getting different batches of brand-name Prograf with wildly different absorption. The system’s always been broken. Now it’s just cheaper. The real villain? The lack of mandatory post-market surveillance for transplant drugs. No one’s tracking this stuff long-term. That’s the scandal.
arun mehta
As someone who works in transplant logistics in India, I can confirm: generic availability saves lives here. Many patients would never afford treatment without it. But we have strict protocols - same manufacturer, monthly monitoring, pharmacist-led education. It’s not about the drug. It’s about the system around it. The U.S. needs structure, not panic.
Patrick Roth
Actually, the EMA’s new rules are pointless. They still don’t require testing in transplant patients - just ‘more data.’ That’s like saying ‘we’ll watch the plane crash more closely next time.’ The real solution? Ban generic switches entirely for NTI drugs. No exceptions.
Jasmine Bryant
Just got my levels back after switching generics - 14.8 ng/mL. My doc said it’s fine. But I’m still nervous. Should I ask for a repeat test next week? I don’t want to be that guy who overthinks everything… but I also don’t want to lose my kidney.