Over half of people with diabetes will develop nerve damage-diabetic neuropathy. It doesn’t come with a warning. One day, your feet feel numb. The next, they burn like they’re on fire. Or maybe your hands go tingly, or you can’t feel your toes when you walk. This isn’t just discomfort. It’s your nerves dying from too much sugar in your blood. And if you don’t act, it gets worse. But here’s the truth: diabetic neuropathy can be slowed. Pain can be reduced. Nerves can even start to heal-if you know what to do.
Why Your Nerves Are Damaging
High blood sugar doesn’t just clog arteries or wreck kidneys. It slowly poisons your nerves. Glucose sticks to nerve fibers like sticky syrup, blocking signals and starving them of oxygen. Over time, the nerves can’t send pain, temperature, or touch signals properly. That’s why you might not feel a blister forming on your foot-or why you feel burning pain even when nothing’s wrong. The damage usually starts in your feet and legs, then moves up. About 60 to 70% of people with diabetes get some form of this. For 16 to 26%, it turns painful. That’s not just tingling. It’s sharp, electric shocks. Aching that won’t quit. Sleepless nights because your skin feels like it’s crawling. And here’s the worst part: once nerves are gone, they don’t come back easily.The Only Thing That Stops It: Blood Sugar Control
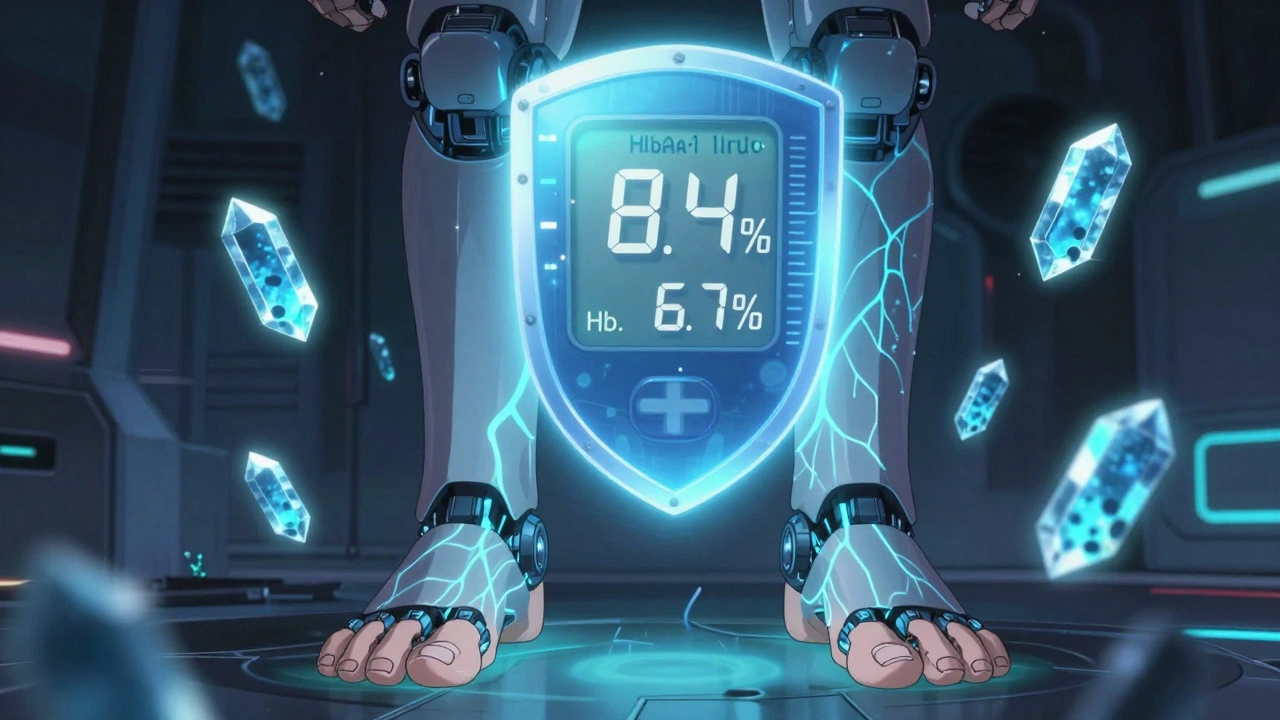
No pill, no cream, no nerve stimulator will fix this if your blood sugar stays high. The single most powerful tool you have is keeping your HbA1c below 7%. That’s not a suggestion-it’s science. The Diabetes Control and Complications Trial showed that tight control cuts neuropathy risk by 60%. That’s not a small win. That’s life-changing. What does that look like in real life? Fasting blood sugar between 80 and 130 mg/dL. After meals, under 180 mg/dL. Not perfect. But consistent. That means counting carbs, not skipping insulin, checking your levels daily, and adjusting food or meds when numbers creep up. It’s hard. But if you’re serious about protecting your nerves, this is non-negotiable. And here’s something surprising: if you get your blood sugar under control and keep it there for a year, some people start to feel better. Numbness fades. Burning lessens. That’s not magic. That’s nerves healing. The more severe the damage, the less likely this is. But even small improvements matter.Medications That Actually Work (And Which Ones to Avoid)
If pain is already here, you need help. Not just aspirin. Not just ibuprofen. Those won’t touch nerve pain-and they’re risky. Long-term NSAIDs raise your chance of heart problems by 10-20% and can wreck kidneys, which you’re already at higher risk for. The real options are targeted:- Duloxetine (Cymbalta): An antidepressant that works on nerve pain. About 35% of people get at least half their pain gone. Side effects? Nausea, dry mouth, fatigue. Starts at 30 mg daily, bumps up to 60 mg.
- Pregabalin (Lyrica): An antiseizure drug repurposed for nerves. Works for 30-40% of users. Can cause dizziness, weight gain, swelling. Often taken 3 times a day.
- Amitriptyline: An old-school tricyclic antidepressant. More effective than newer drugs-up to 63% pain reduction. But it’s heavy. Drowsiness, dry mouth, blurry vision. Avoid if you’re over 65 or have heart issues.
- Topical capsaicin 8% patch (Qutenza): Applied once every 3 months by a doctor. It burns like hell during treatment-but then the pain drops by 30% in 40% of people. No stomach issues. No drowsiness. Great for older adults or those on 5+ meds.
- Lidocaine patches (5%): Stick on painful spots. Safe, no system-wide side effects. Helps with localized burning or shooting pain.

Non-Drug Treatments That Change Everything
Medications help, but they’re not the whole story. Many patients say the real turning point came when they added movement. Walking 30 minutes a day improves nerve function. Swimming and cycling are gentle on feet. Yoga helps with balance and reduces stress-both big factors in pain perception. One study showed people who exercised regularly had 30% less pain progression than those who didn’t. Then there’s TENS: a small device that sends gentle electric pulses through your skin to block pain signals. In one trial, 83% of users saw pain drop from 3.17 to 1.44 on a 5-point scale. Sham treatments? Only 38% improved. It’s cheap. Safe. No side effects. Worth trying. For stubborn cases, doctors now use nerve blocks-shots of numbing medicine near damaged nerves. Relief lasts weeks. Or peripheral nerve stimulation: a tiny device implanted under the skin sends pulses to calm overactive nerves. It’s surgery, but it’s minor. And some patients report not just less pain-but better feeling back in their toes. The most exciting development? Spinal cord stimulation. It’s not just masking pain. People who’ve been numb for years are starting to feel temperature and pressure again. That’s not common. But it’s happening. And it’s changing how we think about neuropathy: not just a curse, but something we can reverse.What to Avoid (And Why)
Don’t ignore your feet. If you can’t feel a blister, it can turn into an ulcer. And ulcers in diabetics can lead to amputation. Check your feet every day. Use a mirror. Feel for warmth, swelling, redness. Wash them. Dry them. Moisturize-no lotions between toes. Wear shoes that fit. Never walk barefoot. Don’t rely on alcohol to numb the pain. It makes nerve damage worse. Don’t smoke. Smoking cuts blood flow to your nerves. It’s like pouring salt on the wound. Avoid high-sugar, processed foods. They spike glucose, which fuels nerve damage. Eat more vegetables, whole grains, lean protein. Omega-3s from fish or flaxseed reduce inflammation. Magnesium and B vitamins (especially B12) support nerve health. Talk to your doctor before starting supplements.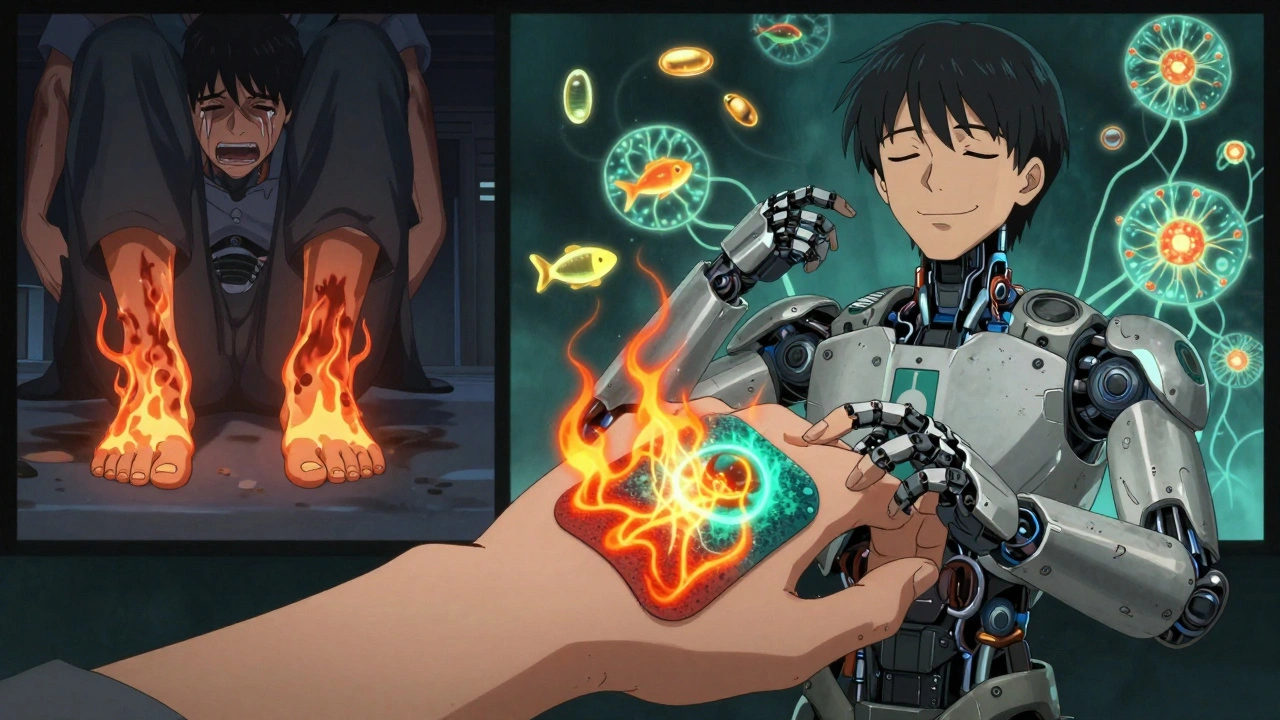
When to See a Specialist
If you’ve tried two or three meds and still can’t sleep or walk, it’s time for a pain specialist. Not just your GP. Look for someone who treats diabetic neuropathy regularly. They’ll know about nerve stimulation, capsaicin patches, and newer options like spinal cord implants. Also, if you’re losing balance, dropping things, or can’t feel your feet when you stand, that’s a red flag. You need a neurologist. They can test nerve function with EMG or skin biopsies to see how bad the damage is. And if you’re feeling hopeless, depressed, or anxious because of the pain-ask for help. One in four people with painful neuropathy develop depression. It’s not weakness. It’s the brain reacting to constant pain. Therapy, antidepressants, or support groups can make a huge difference.Real People, Real Results
Maria, 68, from Sydney, started with burning feet so bad she couldn’t wear socks. She tried duloxetine-made her nauseous. Pregabalin-gained 12 pounds. Then she got the capsaicin patch. One application. No side effects. Pain dropped by 40%. She started walking daily. Within 10 months, her HbA1c went from 8.4% to 6.7%. Her numbness didn’t vanish-but the burning? Gone. She says, “I sleep through the night for the first time in five years.” James, 54, had been on tramadol for two years. He was tired, constipated, and still in pain. His doctor switched him to TENS and a daily 20-minute walk. He dropped the tramadol. Within six months, his pain score halved. He says, “I didn’t need a miracle. I just needed to stop ignoring my feet.”What’s Next?
Scientists are working on drugs that don’t just mask pain-they repair nerves. Nav 1.7 blockers, nerve growth factor antibodies, calcium channel inhibitors-these are in trials. Some may be available in 5 to 10 years. But you don’t have to wait. The tools to protect your nerves and reduce pain are here now. Start with your blood sugar. Then add movement. Then pick one treatment that fits your life. Don’t wait for the perfect solution. The best time to protect your nerves was years ago. The second-best time is today.Can diabetic neuropathy be reversed?
In early stages, yes-partially. If you get your blood sugar under control and keep it there, some nerve function can return. Numbness and tingling may fade within a year. But if nerves are completely dead, they won’t grow back. The goal isn’t to cure it, but to stop it from getting worse and reduce pain enough to live well.
What’s the best medication for diabetic nerve pain?
There’s no single best drug. Duloxetine and pregabalin are FDA-approved and work for many. Amitriptyline is more effective but has stronger side effects. Capsaicin patches are excellent for localized pain with no systemic side effects. The best choice depends on your age, other health conditions, and how your body reacts. Talk to your doctor about trying one at a time.
Can I use ibuprofen for diabetic neuropathy pain?
No. Ibuprofen and other NSAIDs don’t work on nerve pain. They’re designed for inflammation, like arthritis. For diabetic neuropathy, they’re ineffective and risky. Long-term use can damage kidneys and increase heart attack risk-both already higher in people with diabetes. Skip them.
How long does it take for nerve pain to improve after better blood sugar control?
It varies. Some notice less burning within weeks. Others take 6 to 12 months. The key is consistency. If your HbA1c drops and stays low, you’re giving your nerves a chance to heal. Don’t expect overnight results-but don’t give up either. Many people report feeling better after a full year of tight control.
Is exercise safe if my feet are numb?
Yes-but choose wisely. Walking, swimming, cycling, and seated exercises are safe. Avoid high-impact activities like running if you have foot ulcers or severe numbness. Always wear proper shoes. Check your feet before and after. Exercise doesn’t hurt your nerves-it helps them by improving blood flow and lowering blood sugar.
What should I do if my pain gets worse suddenly?
Don’t ignore it. Sudden worsening could mean an infection, a new injury you didn’t feel, or a different condition like a pinched nerve. See your doctor right away. If you have a cut, red spot, or swelling on your foot, treat it like an emergency. Diabetic foot infections can spread fast.
Can I stop taking neuropathy meds if my pain improves?
Only under your doctor’s guidance. Even if pain fades, stopping meds suddenly can cause withdrawal or rebound pain. Your doctor may slowly lower the dose, but don’t quit on your own. Also, keep managing your blood sugar. Pain relief doesn’t mean your nerves are fully healed.
Francine Phillips
ive been dealing with this for years and honestly half the stuff in this post sounds like marketing fluff
my doc gave me pregabalin and i just felt like a zombie
no magic fixes here
Katherine Gianelli
you’re not alone in feeling this way
but hear me out-small steps matter
my mom went from burning feet to walking her grandkids to the bus stop after she got her a1c under 7% and started daily swims
it wasn’t overnight
but it was real
you deserve to feel better, even just a little
Joykrishna Banerjee
ah yes, the classic ‘just control your blood sugar’ sermon
as if we’re all lazy gluttons who don’t know how to count carbs
the real issue is systemic neglect of diabetic care in underfunded clinics
and you’re selling pharmaceutical band-aids like they’re spiritual enlightenment
pathetic
Myson Jones
i appreciate the thoroughness of this post
it’s rare to see such a balanced overview of both pharmacological and non-pharmacological interventions
especially the emphasis on avoiding nsaids and the nuanced discussion of capsaicin patches
thank you for presenting evidence without sensationalism
parth pandya
one thing missing here is benfotiamine
it’s a form of b1 that actually helps with nerve repair
studies show it reduces pain and tingling
not as flashy as qutenza but cheaper and no dr visit needed
ask your doc about it
also spell check ‘sequestial’ in the post lol
Albert Essel
the data presented here is solid and aligns with current clinical guidelines
however, the emotional weight of living with chronic neuropathy is often underrepresented in medical literature
the psychological toll is as real as the physical symptoms
thank you for including mental health as part of the equation
Charles Moore
i’ve seen people try everything-from tums to tdc
what works for one person can wreck another
the key isn’t finding the perfect drug
it’s finding the right combo for your life
and giving yourself grace when progress is slow
you’re not failing if you’re still trying
Gavin Boyne
oh wow
so if i just stop eating bread and walk 30 minutes i’ll magically feel my toes again?
next you’ll tell me yoga fixes insulin resistance
the truth? most of us are already doing the ‘right’ things
and still burning
and still numb
and still getting told to try harder
thanks for the guilt trip, doc
Rashi Taliyan
my sister lost her foot because she didn’t feel the blister
she was 42
you think this is about pain?
it’s about dignity
it’s about not being a burden
it’s about being able to hug your kids without screaming
don’t talk about ‘managing’-talk about surviving
Kara Bysterbusch
the inclusion of real-life testimonials-maria and james-is profoundly impactful
it transforms abstract medical data into lived human experience
and the emphasis on neuroplasticity and nerve regeneration offers a rare glimmer of hope
in a landscape saturated with fatalism, this is a beacon
thank you for writing this with both precision and heart
Rashmin Patel
guys i just want to say that the capsaicin patch is life changing but you have to be ready for the burn like literally it feels like your skin is on fire for 30 mins and you wanna scream but then after 2 days you can feel your toes again and you cry and then you start walking every day and you feel like a new person and also drink turmeric tea and take magnesium and don’t forget to check your feet even if you think you’re fine because one day you’ll miss a cut and then it’s too late so please please please don’t wait like i did 😭🙏🫶
sagar bhute
everyone here is acting like this is a personal failure when it’s clearly the result of a broken healthcare system that lets people go years without proper education
you think the answer is ‘just check your feet’?
what about the person working two jobs and can’t afford glucose strips?
what about the one whose doctor won’t prescribe lyrica because of insurance?
stop blaming patients and fix the system