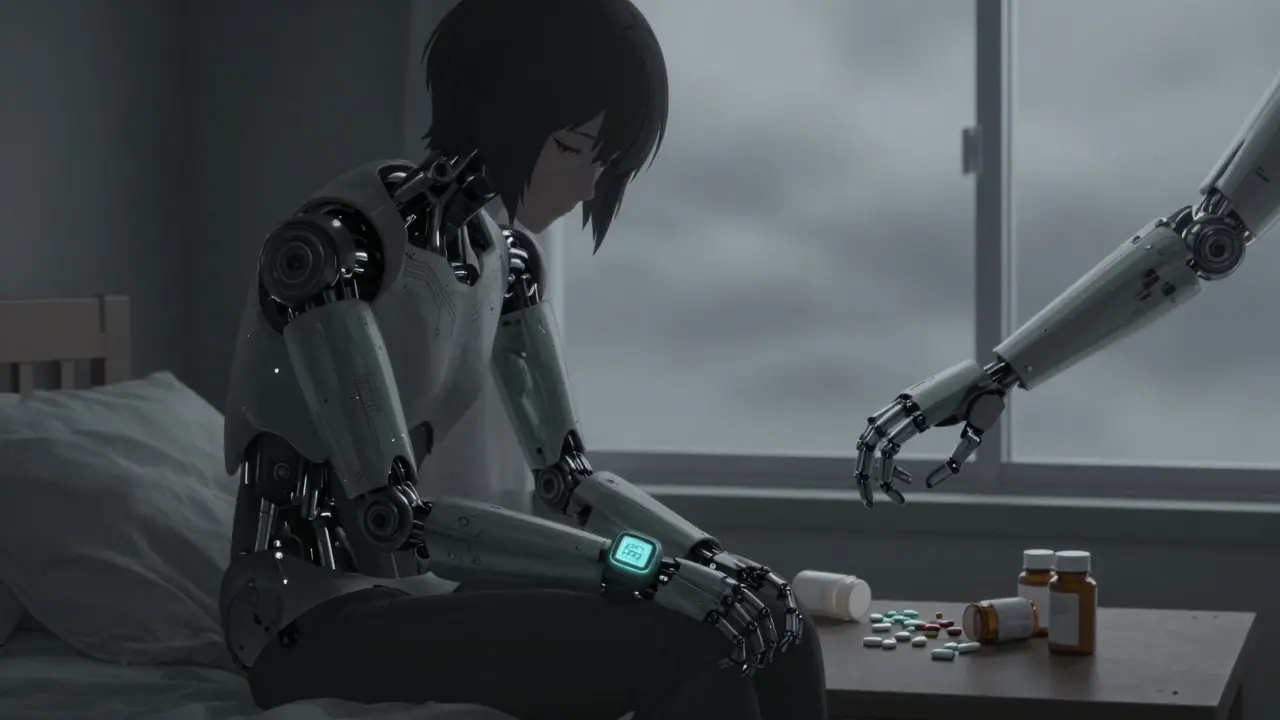
When someone is struggling with depression, taking pills on time isn’t just a habit-it becomes a battle. It’s not about being lazy or forgetful. Depression changes how your brain works, and that directly affects whether you take your medicine as prescribed. This isn’t a small issue. For people with heart disease, diabetes, or even chronic pain, skipping meds because of depression can mean the difference between staying stable and ending up in the hospital.
Depression Doesn’t Just Make You Feel Bad-It Makes You Skip Meds
Research shows clear, measurable links between depression and medication non-adherence. In one major study of heart failure patients, those with depression were 2.3 times more likely to miss their medications than those without depression. That’s not a guess. That’s data from 31 separate studies, adjusted for age, gender, education, and other health conditions. The effect wasn’t random. Depression made people less likely to take ACE inhibitors, beta-blockers, and mineralocorticoid receptor antagonists-all critical drugs for heart health. The higher the depression score, the more likely they were to skip doses.
This isn’t just about the heart. A study from Cambridge University tracked 83 people with major depressive disorder. Using the Morisky Medication Adherence Scale (MMAS-8), they found:
- 39.8% were non-adherent (score below 6)
- 54.2% were only moderately adherent (score below 8)
- Only 6% had perfect adherence (score of 8)
That means nearly 95% of patients with depression weren’t fully taking their meds. And those who skipped the most also had the highest levels of anxiety and stress. Depression doesn’t act alone-it teams up with other mental health struggles to break down adherence.
Why Do People With Depression Skip Their Medication?
It’s not just about forgetting. Depression attacks the mental functions needed to manage treatment. Think about it: you need to remember when to take pills, understand why they matter, plan your day around them, and keep going even when you feel hopeless. Depression steals all of that.
Experts describe three main ways depression gets in the way:
- Cognitive fog: Trouble concentrating, memory lapses, and slow decision-making make complex dosing schedules impossible to follow.
- Amplified side effects: People with depression feel side effects more intensely. A dry mouth or drowsiness from an antidepressant might feel unbearable when you’re already drained. One study found non-adherent patients reported significantly more severe side effects than those who stayed on track.
- Energy drain: Getting out of bed, going to the pharmacy, opening pill bottles-all of it takes effort. Depression saps that energy. Hopelessness whispers, “Why bother?” even when the medicine could save your life.
It’s not defiance. It’s exhaustion. And that’s why telling someone to “just take your pills” doesn’t work.
What Medications Are Most Affected?
Depression doesn’t pick and choose. It affects adherence across the board. But some patterns stand out:
- Antidepressants themselves: Surprisingly, people taking SSRIs like citalopram or sertraline often stop because of side effects-fatigue, weight changes, loss of libido. One study found 83% of those on SSRIs reported non-adherence.
- Heart medications: As shown in the Pizzolorusso review, beta-blockers and ACE inhibitors saw the clearest drop-off in adherence linked to depression scores.
- Diabetes and blood pressure drugs: These often require daily, precise timing. Depression makes routine management nearly impossible.
Even when patients say they’re “doing fine,” depression quietly undermines their ability to stick with treatment. A JAMA Internal Medicine study found that even among groups with high overall adherence, those with depression still missed more doses than others.
How Clinicians Can Spot the Problem
You don’t need fancy tools to recognize this. But you do need to ask the right questions-and measure the answers.
The PHQ-9 is the most widely used depression screen. A score of 10 or higher means moderate to severe depression. For every 5-point increase on the PHQ-9, adherence drops by about 23%. That’s a direct, usable number. If a patient scores 15, expect serious adherence issues.
Pair that with the MMAS-8, an 8-question tool that rates adherence from 0 to 8:
- Score 8 = high adherence
- Score 6-7 = moderate adherence
- Score below 6 = non-adherent
Doctors at Columbia University found that using PHQ-9 and MMAS-8 together improved prediction of non-adherence by 37%. That’s huge. One screen tells you how bad the depression is. The other tells you how much it’s hurting treatment.
Early warning signs matter too. The STAR*D trial showed that if a patient misses more than 20% of their doses in the first two weeks of treatment, they’re nearly five times more likely to have treatment failure. That’s not a coincidence. It’s a red flag.
Real Tools That Work in Practice
Some clinics are already using smart systems:
- Side effect mapping: Patients track daily mood and side effects on a simple chart. Over time, patterns emerge-like “I skip my pill every time I feel too tired.” This helps both patient and doctor see the connection.
- Collaborative care models: In the MAPDep study, patients and doctors reviewed adherence together every few weeks. This simple step boosted adherence by nearly 30% over a year.
- Digital tools: New smartphone apps that track mood and pill intake are showing 82% accuracy in predicting missed doses 72 hours ahead. This isn’t sci-fi-it’s happening now.
The American Heart Association now recommends that heart failure clinics screen every patient with the PHQ-2 (two quick questions) at every visit. If positive, follow up with PHQ-9 and MMAS-8. It’s simple. It’s fast. And it saves lives.

What This Means for You
If you or someone you care about is dealing with depression and a chronic illness, here’s what you need to know:
- Missing pills isn’t a character flaw. It’s a symptom.
- Ask your doctor for a PHQ-9 and MMAS-8 screen. Don’t wait until you’re in crisis.
- Keep a simple log: write down how you felt each day and whether you took your meds. Look for patterns.
- Side effects are real. Talk to your doctor-not about quitting, but about adjusting.
- Help isn’t just about more pills. It’s about better support, better communication, and better systems.
Depression doesn’t care how important your medicine is. It makes everything feel heavy. But recognizing the link between your mood and your meds is the first step to fixing it. You’re not failing. Your brain is just working differently. And with the right tools, you can get back on track.
Can depression cause someone to stop taking their medication even if it’s working?
Yes. Depression doesn’t judge effectiveness-it amplifies discomfort. Even if a medication is helping, side effects like fatigue, dry mouth, or weight gain can feel unbearable to someone with depression. The brain’s ability to weigh long-term benefits against short-term discomfort is impaired. This is why people often stop meds that are working, not because they’re irrational, but because depression distorts their perception of risk and reward.
Is forgetfulness the main reason people with depression miss doses?
No. While memory issues play a role, the bigger factors are lack of motivation, hopelessness, and amplified side effects. A person may remember perfectly well when to take their pill but feel too drained or hopeless to do it. Others avoid taking meds because they associate them with feeling worse, even if the meds are helping. It’s emotional, not just cognitive.
What’s the best way to screen for depression’s effect on medication adherence?
Use the PHQ-9 for depression screening and the MMAS-8 for adherence. Together, they’re far more accurate than either alone. A PHQ-9 score of 10 or higher should trigger an MMAS-8 assessment. Studies show this combination predicts non-adherence 37% better than using one tool by itself. Many clinics now use this dual-screen approach as standard practice.
Do all antidepressants cause adherence problems?
Not all, but many do. SSRIs like sertraline and escitalopram often cause side effects such as drowsiness, weight changes, or loss of libido-side effects that are harder to tolerate when someone is already depressed. Studies show up to 83% of people on SSRIs report non-adherence. The key isn’t avoiding antidepressants-it’s choosing ones with fewer side effects for the individual and monitoring closely from the start.
Can digital tools help track adherence in depressed patients?
Yes. Emerging smartphone apps that link mood tracking with pill reminders have shown 82% accuracy in predicting missed doses 72 hours in advance. These tools work because they capture patterns-not just whether a pill was taken, but how the person was feeling before and after. For someone with depression, seeing the connection between low mood and skipped doses can be a powerful motivator to change.
How long does it take to see improvement in adherence after treating depression?
Improvement can start within weeks. The Frontiers in Public Health study showed that patients in collaborative care programs-where depression and adherence were treated together-had significant improvements in both mood and adherence within 12 weeks. The key is integrated care: treating the depression while actively supporting medication routines, not waiting for one to fix the other.
What Comes Next
If you’re a patient, start by asking your doctor for the PHQ-9 and MMAS-8. If you’re a caregiver, pay attention to patterns-not just missed pills, but how the person talks about their health. Are they saying, “I don’t feel like it,” or “It makes me feel worse”? Those are signs.
The science is clear: depression and medication adherence are linked. Ignoring one while treating the other doesn’t work. The solution isn’t more reminders or alarms. It’s understanding. It’s compassion. And it’s using the right tools to see what’s really going on beneath the surface.
Rachidi Toupé GAGNON
This hit different 😊 Seriously, depression doesn’t care if your meds are life-saving - it just whispers, 'Why bother?' and you’re too tired to argue. I’ve been there. Not lazy. Just drained. But hey - small wins count. Took my pill today? Win. Got out of bed? Double win. You’re not failing. You’re fighting.
PS: If you’re reading this and feeling it - you’re not alone. I’m rooting for you. 🙌
Vamsi Krishna
Let me tell you something. This whole 'depression causes non-adherence' narrative is overblown. I’ve seen patients who skip meds because they’re lazy, not because they're 'depressed.' It’s a convenient excuse. Why not just set alarms? Why not use pill organizers? It’s not rocket science. You’re telling people they’re helpless? That’s the real problem - infantilizing them. They need discipline, not sympathy.
And don’t get me started on those apps. 82% accuracy? Sounds like a startup pitch. Real medicine doesn’t need a smartphone to work.
Brad Ralph
So depression is just a glitch in the human OS? Cool. So we’re saying the brain’s firmware needs an update. 🤔
Meanwhile, doctors are still asking, 'Did you take your pill?' like it’s a quiz. Meanwhile, the patient is thinking, 'I don’t have the emotional bandwidth to care.'
Maybe the real issue isn’t adherence - it’s that we treat chronic illness like a to-do list. It’s not. It’s a grief process. And grief doesn’t follow schedules. Just saying.
christian jon
I can’t believe we’re still having this conversation! PEOPLE ARE DYING BECAUSE WE’RE TOO SOFT TO CALL IT WHAT IT IS! It’s not ‘cognitive fog’ - it’s WEAKNESS! You think your brain is ‘working differently’? NO. It’s choosing to quit. And we’re rewarding that with apps, charts, and ‘collaborative care’? That’s not care - that’s enabling!
My grandfather took his pills at 80 with a broken hip and no family. He didn’t have a PHQ-9. He had grit. Where’s the grit now? Where’s the accountability?
STOP MAKING EXCUSES. START MAKING CHOICES.
Suzette Smith
I mean... I get the science, but isn’t it weird how we always assume depression is the villain? What if the meds are the problem? Like, what if the side effects are actually making people feel worse? Maybe they’re not skipping because they’re depressed - maybe they’re depressed because the pills are making them feel like zombies?
Just saying. Maybe we need to flip the script.
Pat Mun
I’ve spent over a decade working with patients who are managing chronic illness and depression, and I can tell you - this post nails it. It’s not about willpower. It’s not about discipline. It’s about neurobiology. When your brain is drowning in cortisol and serotonin imbalance, even the simplest tasks feel like climbing Everest in a snowstorm. The pill bottle isn’t ignored because you’re lazy - it’s ignored because your nervous system is screaming for survival. And here’s the thing: you don’t need to be fixed. You need to be seen. That’s why collaborative care works - because it doesn’t treat depression and medication separately. It treats the whole person. I’ve seen people go from missing 90% of doses to 95% adherence just by having someone sit with them and say, ‘Tell me what it feels like.’ Not ‘Why didn’t you take it?’ - ‘Tell me what it feels like.’ That’s the magic. Not apps. Not scores. Connection. And yes, it takes time. But change? It starts with being heard.
andres az
Let’s be real - this whole ‘depression = non-adherence’ framework is a symptom of the biopsychosocial model’s collapse. The real issue is pharmaceuticalization of human suffering. We’ve turned emotional distress into a compliance metric. PHQ-9? MMAS-8? These aren’t diagnostic tools - they’re surveillance instruments designed to optimize adherence rates for Big Pharma. The data is cherry-picked. The studies are funded by drug manufacturers. And now we’re telling patients they need digital trackers to prove they’re not ‘non-compliant’? That’s not healthcare. That’s behavioral engineering.
athmaja biju
In India, we don’t have apps or PHQ-9s. We have mothers who wake up at 5 AM to make sure their son takes his pills. We have families who walk 10 kilometers to the clinic because there’s no pharmacy nearby. We don’t talk about ‘cognitive fog.’ We talk about ‘duty.’ You can’t measure hope with a scale. You live it. This post feels very Western. Very clinical. Very detached. In our culture, medicine isn’t taken because it’s convenient - it’s taken because someone loves you enough to remind you. Maybe the solution isn’t tech. Maybe it’s community.
Craig Staszak
I like how this post doesn’t just blame the patient. That’s rare. Most docs just say ‘you’re non-adherent’ and move on. But here? They’re asking why. And that’s the first step. I’ve worked in primary care for 15 years. The moment you stop treating adherence like a compliance issue and start treating it like a communication problem - everything changes. One patient told me, ‘I don’t take my BP pill because it makes me feel like I’m dying.’ Turns out he was having panic attacks from the side effects. We switched meds. He’s been on track for 2 years. No app. No screen. Just a conversation. That’s all it took.
alex clo
The data presented here is robust and aligns with clinical observations in both primary care and specialty settings. The integration of PHQ-9 and MMAS-8 is not merely recommended - it is becoming a standard of care in accredited clinics. The 37% improvement in predictive accuracy is statistically significant and clinically meaningful. Furthermore, the STAR*D trial’s 20% threshold for early non-adherence is a validated predictor of treatment failure across multiple cohorts. This is not speculation. It is evidence-based practice.
Alyssa Williams
I just want to say - if you’re reading this and you’re struggling, you’re doing better than you think. Taking a shower today? Win. Opening the pill bottle? Win. Even thinking about it? Huge win. I used to skip my meds for weeks and feel like garbage. Then I started writing one word in my phone every day: ‘still here.’ That’s it. Just two letters. But it reminded me I hadn’t given up. And slowly? I started taking the pills again. Not because I was ‘fixed.’ But because I was still here. And that’s enough.