When your urine looks foamy and your ankles swell up for no reason, it’s easy to blame a bad night’s sleep or too much salt. But if the swelling doesn’t go away-especially around your eyes in the morning-and you’ve lost 10 pounds in a week without trying, something deeper might be wrong. That’s often how nephrotic syndrome shows up. It’s not a disease on its own. It’s your kidneys screaming that something’s broken inside them.
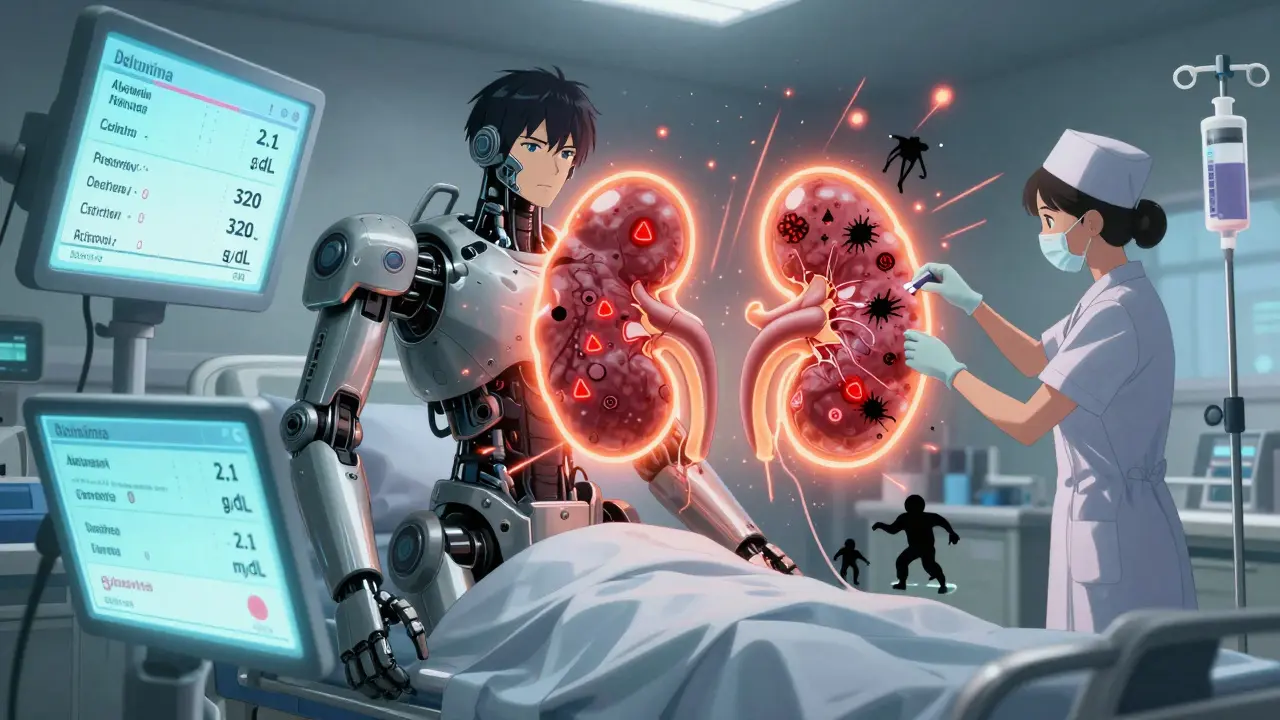
What Exactly Is Nephrotic Syndrome?
Nephrotic syndrome happens when the filters in your kidneys-called glomeruli-get damaged. These filters are supposed to keep protein in your blood. When they’re ruined, protein leaks out into your urine. That’s called proteinuria. In severe cases, you lose more than 3.5 grams of protein every day. That’s like dumping a tablespoon of protein powder into your toilet every 24 hours.
This massive protein loss triggers a chain reaction. Your liver tries to make up for the loss by pumping out more fats, which is why cholesterol levels often shoot above 300 mg/dL. Your blood loses its ability to hold onto water, so fluid leaks into your tissues. That’s the edema-the puffiness around your eyes, swollen legs, or even fluid in your belly. It’s not just uncomfortable. It can make breathing hard if fluid builds up in your lungs.
Doctors don’t diagnose this based on symptoms alone. They need proof: a 24-hour urine test showing over 3.5 grams of protein, blood tests showing albumin below 3.0 g/dL, and cholesterol above 200 mg/dL. No fever, no high blood pressure-those point to something else. Nephrotic syndrome is quiet. It creeps in. That’s why so many parents think their child’s puffy eyes are allergies. The average delay in diagnosis? Seven to ten days.
Why Does This Happen? The Real Causes
There’s no single cause. What triggers it depends on your age.
In kids under six, it’s almost always minimal change disease. The kidneys look normal under a microscope, but the filters are leaking like a sieve. It’s mysterious-no infection, no autoimmune trigger. Just… broken. And here’s the good news: 80 to 90% of these kids respond to steroids within four weeks. They bounce back. But 60 to 70% will have at least one relapse, often after a cold or flu.
In adults, it’s more complicated. The top three culprits are:
- Focal segmental glomerulosclerosis (FSGS)-about 40% of cases. Scarring in patches of the kidney filters. Hard to treat. Often leads to long-term damage.
- Membranous nephropathy-30%. The immune system attacks the kidney filters. Sometimes linked to hepatitis, lupus, or even cancer.
- Diabetic nephropathy-20 to 30%. High blood sugar slowly destroys the filters over years. This is the most common cause in adults over 65.
Then there are the rare ones: genetic forms like congenital nephrotic syndrome, where babies are born leaking protein at over 10 grams a day. Or drug-induced cases from NSAIDs or penicillamine. And autoimmune diseases like lupus can sneak in and cause it too.
Here’s what separates nephrotic syndrome from nephritic syndrome: nephritic syndrome has blood in the urine, high blood pressure, and red blood cell casts. Nephrotic? Foamy urine, swelling, no blood. Two different problems. Confusing them can delay treatment.
How Is It Treated? Beyond Steroids
For children with minimal change disease, prednisone is the go-to. Dosed at 60 mg per square meter of body surface area (up to 80 mg total), given daily for 4 to 6 weeks. Then slowly tapered over months. Most kids go into remission fast. But the side effects? They’re real. Increased hunger, moon face, mood swings, weight gain. One parent on a patient forum said their child gained 15 pounds in six weeks-just from the medicine.
Adults don’t respond as well. Only 60 to 70% get full remission with steroids. And relapses are common-up to 60% of adults will have another flare. That’s where second-line drugs come in.
Calcineurin inhibitors like tacrolimus or cyclosporine are used when steroids fail. They suppress the immune system differently. They work for about half of steroid-resistant cases. But they’re expensive-$1,200 to $2,500 a month-and can damage the kidneys over time if not monitored closely.
ACE inhibitors and ARBs (like lisinopril or losartan) aren’t just for blood pressure. They’re critical for everyone with nephrotic syndrome. They cut protein loss by 30 to 50%. The goal? Keep blood pressure under 130/80. That’s not optional. It’s protective.
And then there’s rituximab. A drug originally for lymphoma, now used for stubborn cases of FSGS and membranous nephropathy. It wipes out the immune cells that attack the kidneys. One study showed it cut proteinuria by 50% in adults who didn’t respond to anything else. But it’s given as an IV infusion-four doses over a month-and costs thousands.
Newer drugs are coming. Sparsentan, approved in 2023, is a dual blocker that targets both angiotensin and endothelin. In trials, it cut proteinuria by nearly 48%-more than double the reduction seen with older drugs. And budesonide (Tarpeyo), originally for IGA nephropathy, is showing promise in some FSGS patients too.
Diet and Lifestyle: What Actually Helps
Medication isn’t the whole story. What you eat matters just as much.
Sodium is the enemy. Too much salt makes swelling worse. The goal? Less than 2,000 mg a day. That means no processed food, no canned soups, no soy sauce. Even bread has hidden salt. One study showed cutting sodium reduced edema by 30 to 50% in just 72 hours.
Protein intake needs balance. Too little and your body starts breaking down muscle. Too much and you stress your kidneys. The sweet spot? 0.8 to 1.0 gram of protein per kilogram of body weight. For a 70 kg adult, that’s about 56 to 70 grams a day-roughly two chicken breasts and a cup of lentils.
Cholesterol is another issue. Statins are often prescribed, but diet helps too. Swap saturated fats for olive oil, nuts, and fatty fish. Avoid fried food and pastries. You’re not just managing numbers-you’re protecting your heart.
And don’t forget vaccines. Live vaccines like MMR or chickenpox are dangerous during steroid treatment. But flu shots, pneumonia shots, and hepatitis B vaccines? Crucial. Your immune system is down. You’re vulnerable.
The Hidden Danger: Blood Clots
Most people don’t know this: nephrotic syndrome makes you 2 to 4 times more likely to get a blood clot. Why? You lose proteins that prevent clotting. Your blood gets sticky.
Renal vein thrombosis-a clot in the kidney’s main vein-is the most common. It can cause sudden back pain, swelling, and even kidney failure. In adults with albumin below 2.0 g/dL, the risk jumps to 10 to 40%. Doctors often prescribe low-dose blood thinners like warfarin or rivaroxaban during the worst phases. It’s not routine for everyone. But if you’re swollen, bedridden, and have low albumin? Ask about it.
Monitoring Progress: What Remission Really Means
Remission isn’t just feeling better. It’s measurable.
For kids, doctors look at urine dipstick tests. Three days in a row of negative or trace protein? That’s remission. Two+ or three+ for three days? Relapse. Parents are taught to test daily during active disease. It’s not optional.
Adults get 24-hour urine collections every few weeks. The goal? Get proteinuria under 1 gram per day. If you’re still over 1 gram after six months of treatment, your risk of kidney failure jumps 4.2 times.
Long-term outlook? It depends on the cause:
- Minimal change disease: 95% of patients keep their kidneys working 10 years later.
- FSGS: Only 50 to 70% make it that far.
- Diabetic nephrotic syndrome: 40 to 50% survival at 10 years.
That’s why early, aggressive treatment isn’t just about feeling better. It’s about keeping your kidneys alive.
What’s Next? The Future of Treatment
Research is shifting from one-size-fits-all to precision medicine. The NEPTUNE study found three distinct molecular subtypes of FSGS. Some respond to steroids. Others need different drugs. Genetic testing is now recommended for kids under one or with a family history. Why? Because if it’s a gene mutation like NPHS1, steroids won’t help-and you don’t want to give them for nothing.
Scientists are now testing drugs that protect podocytes-the actual cells that form the kidney filter. Rho kinase inhibitors, for example, have cut proteinuria by 60 to 70% in animal models. Human trials are coming.
One thing’s clear: nephrotic syndrome isn’t a death sentence. But it’s not something you can ignore. The sooner you treat it, the better your kidneys will last.
Is nephrotic syndrome the same as kidney failure?
No. Nephrotic syndrome is a symptom of kidney damage, not the end stage. Many people with it never develop kidney failure, especially if treated early. But if proteinuria stays high for years-over 1 gram per day-the risk of progressing to end-stage kidney disease increases dramatically. The goal of treatment is to prevent that progression.
Can children outgrow nephrotic syndrome?
Yes, especially with minimal change disease. Most children who respond to steroids will have their last relapse by their teenage years. By age 18, about 80% are in permanent remission. But some will have occasional flares into adulthood. The key is managing relapses early and avoiding triggers like infections.
Why does my urine look foamy?
Foamy urine happens because of excess protein. Normally, your urine is clear or pale yellow. When large amounts of albumin leak into it, the surface tension changes, creating bubbles that don’t pop quickly. It’s not normal foam like soap-it’s persistent, fine bubbles. If you notice this for more than a few days, get it checked.
Are there natural remedies for nephrotic syndrome?
There’s no proven natural cure. Supplements, herbs, or detox diets won’t fix the damaged kidney filters. But diet and lifestyle support treatment. Reducing salt, eating enough protein, controlling cholesterol, and avoiding NSAIDs help. But they’re not replacements for medication. Always talk to your nephrologist before trying anything new.
How often do I need to see a specialist?
During active disease, you’ll likely see a nephrologist every 2 to 4 weeks. Once in remission, visits drop to every 3 to 6 months. Adults average 4.7 specialist visits per year. Regular monitoring catches relapses early and prevents complications like clots or infections. Skipping appointments increases the risk of permanent kidney damage.
Can I still exercise with nephrotic syndrome?
Yes, as long as you’re not severely swollen or feeling dizzy. Light to moderate activity-walking, swimming, yoga-is encouraged. It helps with circulation, reduces swelling, and improves mood. Avoid heavy lifting or intense workouts if you’re on blood thinners or have high blood pressure. Always check with your doctor before starting a new routine.
What to Do Next
If you’ve been diagnosed, start with the basics: track your urine with dipsticks, cut salt, take your meds, and go to every appointment. Don’t wait for swelling to get worse. Don’t assume steroids are the only option. Ask about ACE inhibitors, about genetic testing, about newer drugs like sparsentan.
If you’re a parent and your child has puffy eyes, don’t wait. Get a urine test. Early treatment means fewer relapses, less steroid exposure, and a better chance at a normal life.
Nephrotic syndrome is serious. But it’s not hopeless. With the right care, most people live full, active lives. The key? Don’t ignore the signs. Act fast. Stay consistent. Your kidneys are counting on it.

jenny guachamboza
I heard the FDA is hiding the truth about nephrotic syndrome... it's actually caused by 5G towers messing with your kidney's WiFi signal. 📶💀 I know a guy who swapped his meds for a copper hat and now his proteinuria is 'balanced'... whatever that means.
Sam Black
There's something quietly beautiful about how the body tries to heal itself-even when the system fails. The kidneys, these silent poets, keep whispering through protein leaks and swollen ankles. We treat symptoms like enemies, but maybe they're just messengers. Slow down. Listen. The body doesn't lie.
Tony Du bled
Man, I had a cousin go through this. Puffy eyes for months, doc thought it was allergies. Turned out he was dumping protein like a broken faucet. Started on steroids, gained 30 lbs, looked like a moon bear. But he's been in remission for 5 years now. Just don't skip the follow-ups. It's not a 'take a pill and forget' thing.
Kathryn Weymouth
The distinction between nephrotic and nephritic syndrome is critical-and often misunderstood. Nephrotic syndrome presents with heavy proteinuria, hypoalbuminemia, edema, and hyperlipidemia; nephritic syndrome includes hematuria, hypertension, and RBC casts. Confusing the two leads to mismanagement. This post accurately delineates these entities. Well-researched.
Nader Bsyouni
They say steroids fix minimal change disease but what if the real problem is the industrial food supply poisoning our podocytes? Glyphosate in your bread your oatmeal your soy sauce it's all connected and no one wants to talk about it because Big Pharma profits off the cycle of relapse and re-treatment
Julie Chavassieux
I swear my kid’s puffy eyes were just from crying after his Xbox got taken away… until the doctor said ‘proteinuria’ and I nearly fainted. Now I’m Googling ‘is nephrotic syndrome a government mind control experiment’ at 3am. HELP.
Herman Rousseau
This is one of the clearest explanations I’ve seen. Seriously. If you’re reading this and you or someone you love is dealing with this-don’t panic. You’re not alone. Track your urine, cut the salt, take your meds, and find a good nephrologist. It’s a marathon, not a sprint. And yes, you can still hike, swim, laugh, live. 💪❤️
Ajay Brahmandam
In India, many don’t even get tested till they’re swollen like balloons. My uncle had FSGS and couldn’t afford tacrolimus. He survived on low-salt diet and prayer. We need cheaper access to these drugs. Sparsentan sounds amazing but who can afford it?
Cara Hritz
I think the real issue is that doctors dont understand how much stress affects the kidneys like at all like I had a total breakdown last year and then my proteinuria spiked like whoa like what even is happening
Jamison Kissh
If the glomeruli are the filters, then what is the soul of the kidney? Is it the podocyte’s will to hold back the flood? Or is it simply chemistry-electrostatic repulsion, structural integrity, molecular gates? We treat it like a machine, but what if it’s more alive than we admit?
Aliyu Sani
Bro, in Lagos, we call this 'water belly' and most folks just use herbal mixtures. Some work, some don't. But the real issue? No labs. No urine dipsticks. If you can't test it, you can't treat it. We need mobile nephro units, not just fancy new drugs.
Gabriella da Silva Mendes
I mean, if you're not from the US, you're basically screwed. Like, good luck getting rituximab if you're on Medicaid. And don't even get me started on how they treat kids in other countries. We're the best. We have the drugs. We have the science. Everyone else is just… waiting.
Kiranjit Kaur
My cousin’s daughter had minimal change disease at 3. She’s 14 now, no meds, no relapses. She plays soccer, does ballet, eats pizza. I cried when I read this. You’re not alone. There’s hope. 🌈💖
Art Van Gelder
You know what’s wild? The body’s got this insane ability to adapt. Protein leaks out? Liver goes into overdrive making lipids. Blood pressure drops? Fluid leaks into tissues to compensate. It’s like nature’s version of a DIY fix-messy, inefficient, but somehow… persistent. We’re just trying to outsmart a system that’s been running for 3 billion years.
Candy Cotton
It is imperative that all patients with nephrotic syndrome adhere strictly to the prescribed therapeutic regimens, as noncompliance may precipitate irreversible renal parenchymal damage. Furthermore, the consumption of sodium in excess of two grams per day constitutes a significant impediment to therapeutic efficacy. The medical literature is unequivocal on this point.