Pioglitazone Safety Risk Assessment
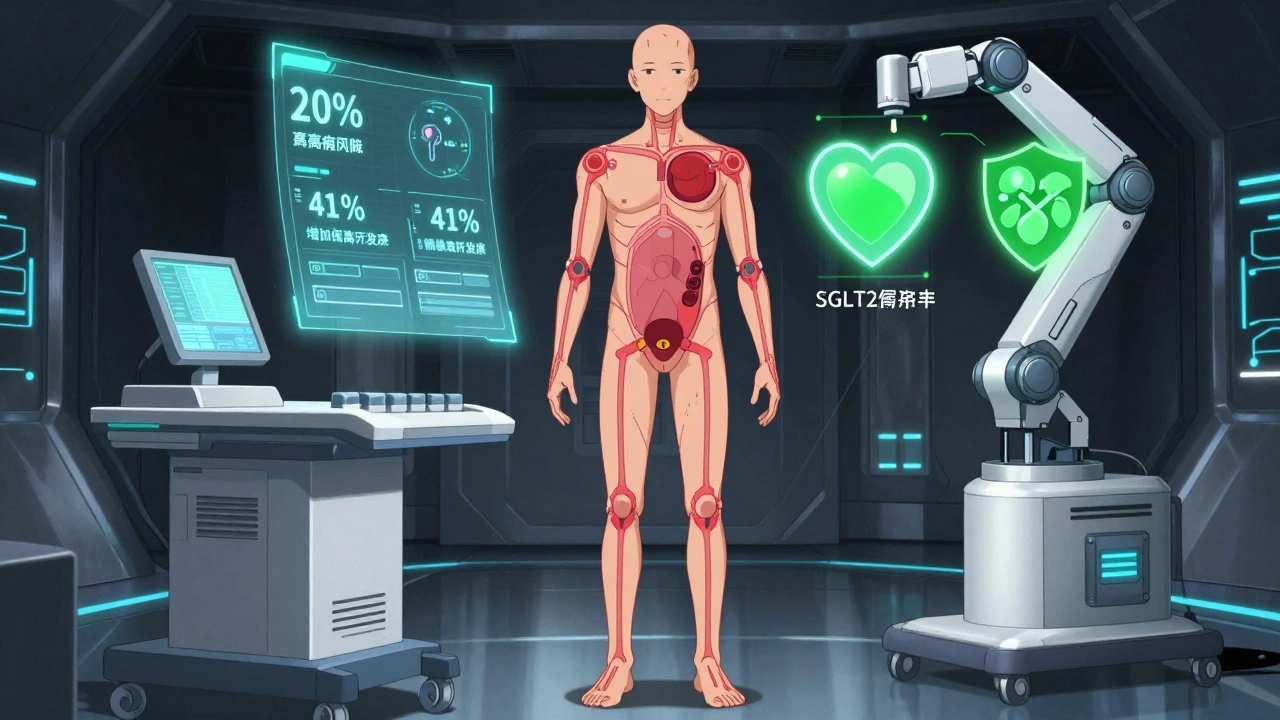
This tool helps you understand your personal risk profile for complications associated with pioglitazone (ACTOS). Based on medical guidelines and research data from the article, this assessment identifies your risk level for heart failure, edema, and bladder cancer.
When you're managing type 2 diabetes, finding a medication that lowers blood sugar without causing new problems is tough. Pioglitazone - sold under the brand name ACTOS - was once a go-to drug for improving insulin sensitivity. But over the last decade, its use has dropped sharply. Why? Because for some people, the risks outweigh the benefits. The big concerns? Pioglitazone can cause heart failure, swelling in the legs and feet, and may raise the chance of bladder cancer. These aren’t rare side effects. They’re well-documented, serious, and require careful monitoring.
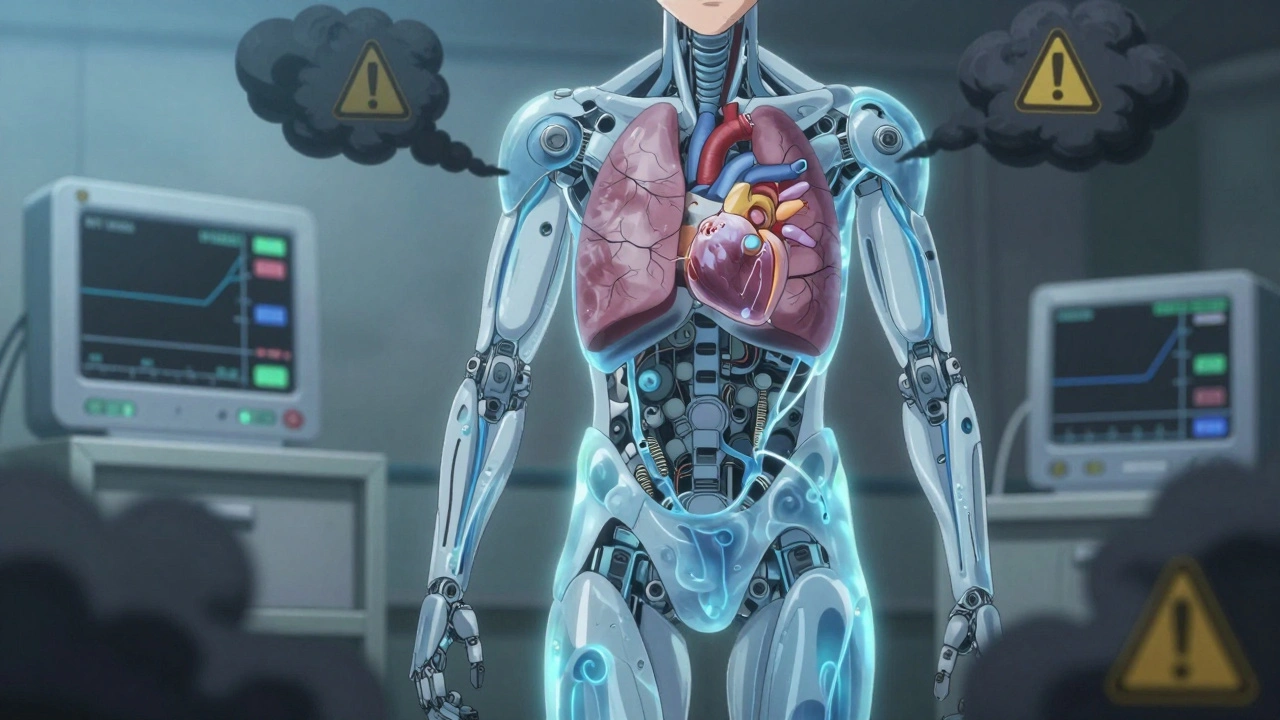
How Pioglitazone Works - and Why It Causes Fluid Retention
Pioglitazone belongs to a class of drugs called thiazolidinediones. It works by activating PPAR-γ receptors, which help your body respond better to insulin. That means lower blood sugar - and that’s the good part. But here’s the catch: this same mechanism causes your body to hold onto extra fluid. Studies show it increases plasma volume by 6-7%. That’s not a small amount. It’s enough to make your ankles swell, your clothes feel tight, and your weight jump by 5-10 pounds in just a few weeks.
This isn’t just water weight you can ignore. That fluid doesn’t just sit in your legs - it can build up in your lungs and heart. In clinical trials, 27% of people taking pioglitazone developed swelling, compared to just 16% on placebo. And in over one-third of cases where heart failure happened, the swelling came first. The problem? Diuretics often don’t help. The only reliable fix? Stopping the drug. Once you stop, the fluid usually drains away in days.
The Heart Failure Risk Is Real - And Not Just for People With Existing Heart Disease
The FDA requires a boxed warning - the strongest kind - for pioglitazone because of heart failure. It’s not just a caution. It’s a hard rule: don’t use it if you have Class III or IV heart failure. That means severe symptoms like shortness of breath while resting, or needing to sleep propped up on pillows.
But even if you don’t have heart failure yet, pioglitazone can push you toward it. A major analysis of over 16,000 patients found that those taking pioglitazone had a 41% higher risk of severe heart failure compared to those on other treatments. The risk jumps even higher if you’re older, have kidney problems, or already have high blood pressure. One study showed that 2.3% of people on pioglitazone ended up hospitalized for heart failure, versus 1.8% on other drugs. That might sound small, but for someone with diabetes already at higher risk for heart issues, it’s significant.
Doctors now avoid prescribing it to anyone with a recent heart failure hospitalization or high levels of NT-proBNP - a blood marker that signals heart stress. If your levels are above 125 pg/mL, pioglitazone is off the table.
Edema Isn’t Just a Nuisance - It’s a Warning Sign
Swelling in the ankles, feet, or hands is the most common side effect of pioglitazone. But many patients don’t realize it’s linked to the drug. They think it’s just aging, standing too long, or eating too much salt. In reality, it’s your body reacting to the medication.
On patient forums, stories are consistent: “I gained 8 pounds in a month - my ankles looked like balloons.” “I couldn’t fit into my shoes.” “I had to quit because I felt like I was drowning.” These aren’t exaggerations. In one study, 21.6% of patients on pioglitazone had edema without heart failure - and that number was nearly double the placebo group.
What makes it dangerous is how easily it’s missed. Weight gain of more than 2-3 pounds in a week? That’s not normal. Shortness of breath when lying down? That’s not just being out of shape. These are red flags. That’s why doctors recommend checking your weight every week for the first two months. If you gain more than 5 pounds in a month, the drug should be re-evaluated - not just adjusted.
Bladder Cancer: A Long-Term Risk That Can’t Be Ignored
While heart failure and swelling are immediate concerns, bladder cancer is the silent threat. In 2011, the FDA issued a warning after analyzing data from the PROactive study - a 10-year trial involving over 5,000 patients. Those taking pioglitazone had a 20% higher risk of developing bladder cancer compared to those on other diabetes meds. The absolute risk is low - about 1 in 100 over 10 years - but it’s real.
That’s why doctors now avoid pioglitazone in patients with a personal history of bladder cancer. It’s also not recommended if you have blood in your urine, frequent urination, or pain when peeing - symptoms that could signal early cancer. The risk increases the longer you take it. After five years, the chance goes up noticeably. That’s why many doctors won’t prescribe it for more than 1-2 years unless absolutely necessary.
It’s worth noting: this risk doesn’t apply to all thiazolidinediones. Rosiglitazone was pulled from the market in Europe over heart concerns, but not bladder cancer. Pioglitazone is the only one with this specific link.
Who Should Still Consider Pioglitazone?
Despite the risks, pioglitazone isn’t completely dead. It still has a role - but only for very specific cases. It’s one of the few drugs that can improve liver fat in people with non-alcoholic steatohepatitis (NASH), a common condition in people with type 2 diabetes. In the PIVENS trial, 53% of patients on pioglitazone showed improved liver tissue - compared to just 24% on placebo.
It’s also useful for patients who can’t tolerate metformin or who have low insulin levels. Unlike sulfonylureas, it doesn’t cause hypoglycemia. Unlike SGLT2 inhibitors, it doesn’t increase the risk of genital infections. So if you’re someone with fatty liver disease, stable heart function, no history of bladder cancer, and you’re willing to be monitored closely, it might still make sense.
But even then, it’s usually a last-resort option. Most endocrinologists now start with metformin, then move to SGLT2 inhibitors or GLP-1 agonists - drugs that not only lower blood sugar but also protect the heart and kidneys. Pioglitazone doesn’t offer that protection. It just manages glucose - with side effects.
What to Do If You’re Currently Taking Pioglitazone
If you’re on pioglitazone, don’t stop cold turkey. Talk to your doctor. But here’s what you should ask:
- Have I been screened for heart failure risk? (Ejection fraction, NT-proBNP levels)
- Do I have any signs of bladder cancer? (Blood in urine, frequent urination)
- Have I gained more than 5 pounds in the last month?
- Do I have swelling in my legs or feet that doesn’t go away?
If you answer yes to any of these, your doctor should consider switching you. The good news? There are better options now. SGLT2 inhibitors like empagliflozin and dapagliflozin actually reduce heart failure hospitalizations. GLP-1 agonists like semaglutide help with weight loss and heart protection. These drugs have fewer side effects and more benefits.
And if you’ve been on pioglitazone for more than two years? That’s a red flag. Most guidelines now recommend limiting use to under two years unless there’s a clear, ongoing benefit that can’t be achieved another way.
Monitoring Is Non-Negotiable
If your doctor still thinks pioglitazone is right for you, you need a strict monitoring plan:
- Baseline ECG and echocardiogram to check heart function
- Urine test to rule out blood in urine
- Weekly weight checks for the first two months
- Monthly blood pressure and leg swelling checks
- Annual bladder cancer screening if you’ve been on it for more than a year
Many clinics now use digital weight logs and symptom trackers. If your weight jumps more than 2 pounds in a week, you get an automatic call from the nurse. That’s how seriously this is taken now.
The Bigger Picture: Why Pioglitazone Use Is Dropping
In 2010, over 18 million prescriptions were written for pioglitazone in the U.S. By 2022, that number dropped to 5.2 million - a 72% decline. Why? Because safer, more effective drugs came along. SGLT2 inhibitors and GLP-1 agonists don’t just control blood sugar - they save lives. They reduce heart attacks, strokes, and hospital stays for heart failure. Pioglitazone doesn’t do that. It just helps glucose - and sometimes breaks your heart.
Even in Europe, where pioglitazone is still available, it’s restricted to second-line use only - after metformin fails, and only if heart and bladder risks are ruled out.
It’s not that pioglitazone doesn’t work. It does. But in 2025, we have tools that work better - and safer. The question isn’t whether pioglitazone helps with blood sugar. It’s whether the trade-off is worth it.
Can pioglitazone cause weight gain even if I’m eating well?
Yes. Pioglitazone causes weight gain primarily through fluid retention, not increased appetite or fat storage. Even if you’re eating the same amount, you can gain 5-10 pounds in a few weeks due to water buildup. This isn’t fat - it’s fluid, and it’s a direct side effect of the drug.
Is pioglitazone still prescribed today?
Yes, but rarely. It’s mostly used in patients with non-alcoholic steatohepatitis (NASH) who haven’t responded to other treatments, or in those who can’t tolerate newer drugs. Most doctors avoid it due to the heart failure and bladder cancer risks. Newer medications like SGLT2 inhibitors are preferred because they offer heart and kidney protection.
How do I know if my swelling is from pioglitazone or something else?
Swelling from pioglitazone usually starts in the ankles and feet, gets worse over days or weeks, and doesn’t improve with diuretics. It’s often accompanied by rapid weight gain (more than 2-3 pounds per week). If you started the drug recently and noticed swelling, it’s likely related. Your doctor can confirm with blood tests and an echocardiogram.
Can I take pioglitazone if I have high blood pressure?
High blood pressure alone doesn’t disqualify you, but it increases your risk of heart failure when taking pioglitazone. If you have high blood pressure and other risk factors - like being over 65, having kidney disease, or a history of heart issues - your doctor will likely avoid pioglitazone. They’ll prefer drugs that lower blood pressure and blood sugar at the same time, like SGLT2 inhibitors.
What are the safest alternatives to pioglitazone for type 2 diabetes?
The safest alternatives are SGLT2 inhibitors (like empagliflozin or dapagliflozin) and GLP-1 receptor agonists (like semaglutide or liraglutide). These drugs lower blood sugar, promote weight loss, reduce heart failure risk, and protect the kidneys. They’ve been shown in large studies to lower the risk of death from heart disease - something pioglitazone doesn’t do. Most guidelines now recommend these as first or second-line options over pioglitazone.
What Comes Next
If you’re on pioglitazone and have concerns, schedule a review with your doctor. Bring your weight logs, note any swelling, and ask about your heart and bladder health. Don’t wait for symptoms to get worse. The goal isn’t just to control blood sugar - it’s to live longer, healthier, and without avoidable complications. There are better options now. You deserve to know what they are.
Jennifer Patrician
So let me get this straight - the FDA says pioglitazone causes heart failure and bladder cancer, but Big Pharma still sells it? Yeah right. They're just using it to keep people hooked on monthly co-pays while they fund lobbyists to block real alternatives. I've seen the documents. They knew. They always knew. And now they're pushing SGLT2 inhibitors like they're miracle drugs - same companies, same playbook. #PharmaLies
Jimmy Jude
The real tragedy isn't the drug - it's the surrender of medical autonomy. We used to treat the whole person. Now we follow algorithmic guidelines written by bureaucrats who've never met a patient. Pioglitazone isn't evil - it's misunderstood. Like all tools, it's only dangerous in the hands of the unwise. And who's unwise? The system that turns healing into a checklist.
Rupa DasGupta
I was on this for 8 months 😭 my feet looked like balloons and I cried every time I tried to put on my favorite shoes... then my doctor said "it's just water weight" and I wanted to scream. I stopped it cold turkey and within 10 days? POOF. Gone. No more swelling. No more panic. I'm not mad at the drug - I'm mad at how NO ONE warned me. 🤕💧
ashlie perry
They say bladder cancer risk is low but what if you're the one in 100? My uncle died from it after 4 years on pioglitazone. They never tested his urine. No one asked. Now they say it's "rare" like that makes it okay. I'm done trusting doctors who don't listen.
Juliet Morgan
Hey - if you're on this med and you're scared, you're not alone. I was too. But you're already doing the right thing by reading this. Talk to your doc. Bring this post. Ask for the NT-proBNP test. Weight logs matter. You deserve to be heard. You're not being dramatic - you're being smart. I believe in you 💪
Harry Nguyen
Of course the government banned it in Europe. They're all socialists who think medicine should be free and safe. Here in America we have real choices. If you want to take a drug that works, even with risks, that's your right. Stop crying about water weight and start taking responsibility. I've been on it for 6 years. No cancer. No heart failure. Just better blood sugar.
Chris Brown
The empirical data is unambiguous. The hazard ratio for congestive heart failure is 1.41 with a 95% confidence interval of 1.27–1.56. Furthermore, the incidence of bladder carcinoma demonstrates a dose- and duration-dependent relationship. To dismiss these findings as anecdotal is to misunderstand the foundational principles of evidence-based medicine.
Stephanie Fiero
I just wanna say to anyone reading this - if you're gaining weight fast and your legs feel heavy, don't wait. Go to urgent care. Tell them you're on pioglitazone. They'll check your BNP and echo. I did. They caught early fluid overload. Saved me from hospitalization. You're not overreacting. You're being proactive. I'm proud of you. 🤍
Laura Saye
The paradigm shift here is not merely pharmacological but ontological. We have moved from a model of symptom management to one of holistic risk mitigation. Pioglitazone, while efficacious in PPAR-γ modulation, operates within a mechanistic framework that inherently exacerbates fluid dynamics and cellular proliferation in epithelial tissues. The newer agents, by contrast, engage pleiotropic pathways - renal, cardiovascular, and metabolic - that confer net benefit. This is not abandonment. It is evolution.