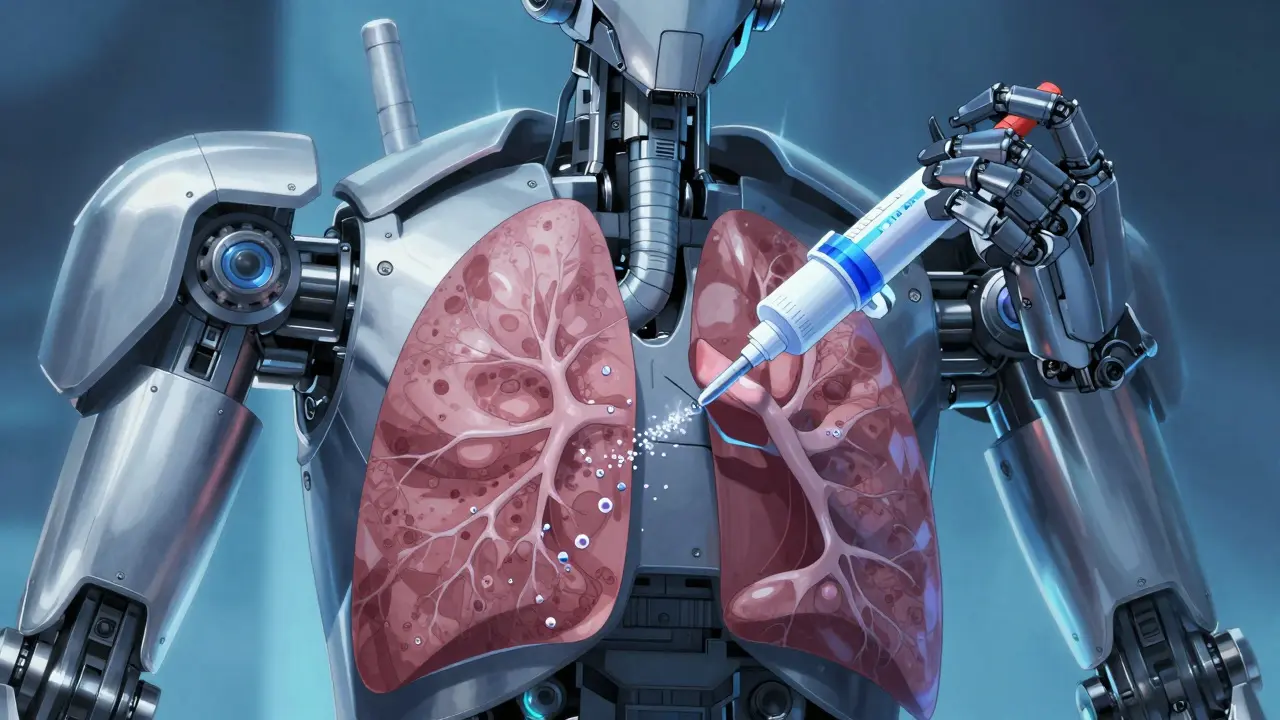
If you or a loved one uses an inhaler for asthma or COPD, there's a good chance you're not using it right. Studies show 70-90% of patients make mistakes that leave most of the medication in the mouth or throat instead of the lungs. That means your treatment isn't working as well as it could.
In inhalers, proper inhaler technique is the key to getting medication where it needs to go. When used correctly, 40-60% of the dose reaches the lungs. But with poor technique, that number drops to just 8-30%. This difference can mean the difference between controlling symptoms and constant breathing trouble.
Why Proper Inhaler Technique Matters
When your inhaler doesn't work as intended, you're not just wasting medication-you're risking serious health complications. The National Heart, Lung, and Blood Institute reports that improper inhaler use leads to more emergency room visits, hospitalizations, and higher medication costs. A 2022 study in the Journal of Asthma found that patients with correct technique had 35% fewer asthma attacks than those who didn't. This isn't just about feeling better today; it's about preventing long-term damage to your lungs.
Imagine taking a full dose of medicine but only getting a fraction of it where it should go. That's what happens when technique is off. For example, if you don't hold your breath after inhaling, up to 20-30% of the medication gets exhaled immediately. Or if you don't shake your metered-dose inhaler before use, the medication settles and delivers uneven doses. These small errors add up to major health impacts over time.
Real-world Impact of Proper Technique
Correct inhaler use isn't just theoretical-it changes lives. A 2023 JAMA Internal Medicine study tracked 12,000 patients over two years. Those who received technique training had 22% fewer emergency room visits and saved $480 per year in healthcare costs. One patient, Maria, had been using her inhaler incorrectly for years. After a pharmacist showed her the right way, her asthma attacks dropped from daily to once a month. "I didn't realize I was wasting medication," she said. "Now I feel like I have my life back."
On the flip side, improper use has serious consequences. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) reports that poor technique contributes to 3.6 million preventable COPD deaths annually. In low-income countries where training is scarce, these numbers are even higher. This isn't just about personal health-it's a public health issue.

How Different Inhalers Work
There are three main types of inhalers, each requiring specific techniques. Understanding how they function helps you use them correctly.
Metered-dose inhalers (MDIs) are the most common. They use a pressurized canister to spray medication when you press the device. The American Lung Association explains that MDIs require precise timing: you must press the canister while inhaling slowly for 3-5 seconds. Without this coordination, up to 70% of the medication ends up in your mouth. Using a spacer with an MDI can improve delivery by 70-100%.
Dry powder inhalers (DPIs) like the Diskus or Turbuhaler work differently. They don't have a propellant-instead, you inhale quickly and forcefully to release the powder. The Cleveland Clinic notes that DPIs require a minimum inhalation flow of 30-60 liters per minute. If you don't inhale fast enough, the powder won't aerosolize properly. This makes DPIs challenging for people with severe COPD who may not generate enough airflow.
Soft mist inhalers like Respimat create a slow-moving mist that stays airborne longer. This gives you more time to inhale correctly. Boehringer Ingelheim's data shows these devices deliver 50% more medication to the lungs than standard MDIs without spacers. However, they still require proper breathing technique to be effective.
Common Mistakes and Fixes
Even with instructions, patients often make the same errors. Here's what to watch for:
- Not shaking MDIs: 45% of patients skip this step. Shaking ensures medication is evenly mixed. Always shake for 5 seconds before use.
- Exhaling into the device: This can clog the inhaler. Always exhale away from the mouthpiece first.
- Incorrect breath-hold: 63% of users don't hold their breath long enough. Hold for 10 seconds after inhaling to let medication settle.
- Using DPIs without enough force: If you don't inhale fast enough, the powder won't release properly. Practice with a piece of paper to feel the required airflow.
- Not waiting between puffs: The American Lung Association recommends waiting 60 seconds between doses to allow medication to distribute.
For those using inhaled corticosteroids, rinsing your mouth after each dose reduces oral thrush risk by 75%. The Chest Journal confirmed this simple step prevents common side effects.
Special Considerations for Seniors and Children
Older adults and children often need adjusted techniques. The National Asthma Council Australia found that 62% of seniors struggle with DPIs due to weaker inhalation strength. For them, MDIs with spacers are usually better. Children under six may need a spacer with a mask for proper delivery.
For older patients, the key is simplicity. The UK Inhaler Group recommends "single breath and hold" technique for MDIs with spacers. This involves taking one deep breath in and holding it for 10 seconds-no complex coordination needed. For children, using a spacer with a face mask ensures the medication reaches the lungs even if they can't form a tight seal with their mouth.
Expert Tips for Better Results
Healthcare professionals emphasize consistent practice. Dr. Emily Pennington of the Cleveland Clinic says, "Practice your technique monthly. Even experienced users slip up. A quick check with your pharmacist can save you from ineffective treatment."
Keep your inhaler at room temperature (20-25°C). Storing it above 30°C reduces efficacy by 15-20%, according to FDA testing. Never store it in the bathroom where humidity can damage the device.
For those with severe COPD, soft mist inhalers may be the best option. Their slow delivery gives more time to inhale correctly. A 2023 study in the European Respiratory Journal showed 45% better symptom control with soft mist inhalers compared to standard MDIs for advanced COPD patients.
How do I know if I'm using my inhaler correctly?
The best way to check is to ask your doctor or pharmacist to watch you use it. They can spot mistakes you might not notice. Many pharmacies offer free technique checks. You can also watch instructional videos from reputable sources like the American Lung Association.
Can I use a spacer with any inhaler?
Spacers work only with metered-dose inhalers (MDIs). They should not be used with dry powder inhalers (DPIs) or soft mist inhalers, as this can block the medication. Always check with your healthcare provider before using a spacer with your specific device.
Why is my inhaler not relieving my symptoms?
There are several reasons: incorrect technique (most common), expired medication, or a need for different treatment. If your inhaler isn't working, contact your doctor immediately. They can check your technique, review your prescription, and adjust your treatment plan.
How often should I clean my inhaler?
Clean your MDI mouthpiece weekly with warm water and let it air dry. For DPIs, wipe the mouthpiece with a dry cloth-never use water as it can damage the powder. Always follow the manufacturer's instructions for your specific device.
What's the biggest mistake people make with inhalers?
The most common mistake is not coordinating the inhalation with the medication release. For MDIs, pressing the canister and inhaling at the same time is tricky. For DPIs, inhaling too slowly prevents proper powder release. Practice with a spacer or ask your pharmacist for a demonstration.