Psychiatric Medication Interaction Checker
Check for Dangerous Interactions
Enter medication names accurately. Include dosage information if known.
Current Medications
Results
When you’re taking more than one psychiatric medication, it’s not just about how each drug works alone-it’s about how they react together. Some combinations can save lives. Others can land you in the hospital-or worse. The truth is, many people on psychiatric meds are unknowingly at risk. It’s not about being careless. It’s about how complex these drugs are, and how little most patients and even some doctors know about what happens when they mix.
Why Psychiatric Drug Interactions Are So Dangerous
Psychiatric medications don’t just affect your mood. They tweak your brain chemistry at a deep, chemical level. They target neurotransmitters like serotonin, norepinephrine, and dopamine. These aren’t just buzzwords-they’re real chemicals that control everything from your sleep and focus to your heart rate and muscle control. When two drugs that affect the same system are taken together, they can amplify each other. Too much serotonin? That’s serotonin syndrome-a life-threatening condition. Too much dopamine blockade? You could develop rigid muscles, fever, and confusion. These aren’t rare side effects. They happen more often than you think. According to the American Association of Psychiatric Pharmacists, 30-50% of adverse drug events in psychiatric care come from interactions between medications. That’s not a small number. That’s a systemic problem. And it’s not just about two psychiatric drugs. It’s about mixing them with over-the-counter painkillers, herbal supplements, or even alcohol.The Big Three: Serotonin, Norepinephrine, and Dopamine
To understand interactions, you need to know which drugs affect which brain chemicals. Serotonin is the most common culprit in dangerous interactions. SSRIs like fluoxetine and sertraline, SNRIs like venlafaxine, and even some painkillers like tramadol all raise serotonin levels. Add an MAO inhibitor like phenelzine, and you’re playing with fire. MAOIs block the enzyme that breaks down serotonin. So when you combine them with an SSRI, serotonin floods your system. Symptoms start with shivering, diarrhea, and confusion-and can quickly turn to high fever, seizures, and organ failure. Mortality rates for severe serotonin syndrome? Between 2% and 12%. Norepinephrine affects your stress response, blood pressure, and alertness. TCAs like amitriptyline and SNRIs like duloxetine boost it. Combine them with decongestants like pseudoephedrine (found in cold medicines), and your blood pressure can spike dangerously. Add alcohol? That’s a double hit-both depress your central nervous system, increasing dizziness, falls, and even respiratory depression. Dopamine is targeted by antipsychotics like risperidone and olanzapine. These drugs block dopamine to reduce hallucinations and delusions. But if you mix them with other dopamine blockers-like metoclopramide (used for nausea)-you can trigger severe movement disorders. Think muscle rigidity, tremors, and a condition called neuroleptic malignant syndrome, which can be fatal if not caught fast.High-Risk Combinations You Need to Know
Here are the combinations that cause the most emergencies:- SSRI + MAOI: This is the classic deadly combo. Never mix them. Even if you’ve stopped one, you must wait at least 14 days before starting the other. Fluoxetine (Prozac) lingers in your system for weeks-so waiting 5 weeks is safer.
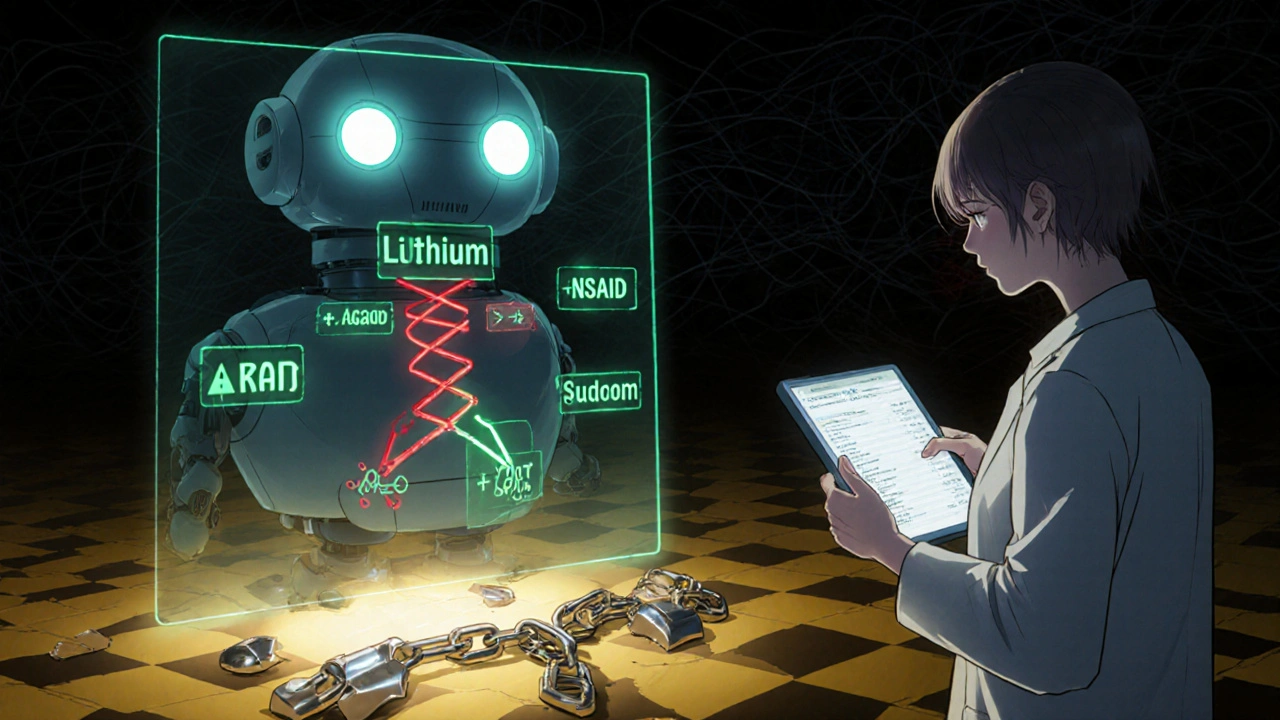
- Lithium + NSAIDs: Lithium treats bipolar disorder, but its therapeutic range is razor-thin: 0.6 to 1.0 mmol/L. NSAIDs like ibuprofen or naproxen can raise lithium levels by 25-50%. One extra painkiller, and you’re in toxicity territory-tremors, vomiting, seizures.
- TCAs + Antihistamines: Both have anticholinergic effects. Combine them, and you get dry mouth, blurred vision, constipation, urinary retention, and rapid heartbeat. In older adults, this can trigger confusion or even delirium.
- Quetiapine + CYP3A4 inhibitors: Drugs like ketoconazole or clarithromycin slow down how your body breaks down quetiapine. Levels build up, increasing sedation, low blood pressure, and heart rhythm problems.
- Fluvoxamine + any drug metabolized by CYP1A2, 2C19, or 3A4: Fluvoxamine is one of the strongest enzyme inhibitors among SSRIs. It can spike levels of clozapine, theophylline, caffeine, and even some blood thinners like warfarin. INR levels can jump 20-30%, raising bleeding risk.

Why Some Medications Are Safer Than Others
Not all psychiatric drugs are created equal when it comes to interactions. Some are like ticking bombs. Others are relatively quiet. For example, sertraline and citalopram have lower interaction potential than fluvoxamine or paroxetine. That’s why many psychiatrists choose them when patients are already on multiple meds. Similarly, vilazodone affects only serotonin with little to no impact on liver enzymes-making it a safer option in polypharmacy. Atypical antipsychotics vary too. Quetiapine has a lower risk profile than risperidone or aripiprazole. Aripiprazole is a partial agonist, which means it doesn’t fully block dopamine-it modulates it. That can mean fewer side effects and fewer dangerous combos. Even newer drugs like brexanolone (for postpartum depression) and cariprazine (for bipolar depression) have been studied for interactions, and their profiles are now included in updated clinical guidelines. But because they’re newer, fewer doctors know how to use them safely.What Doctors Should Be Doing-But Often Don’t
The American Association of Psychiatric Pharmacists (AAPP) has clear guidelines. Yet many clinicians still don’t follow them. Here’s what should happen every time a new psychiatric med is added:- Check the neurotransmitter profile: Use tools like the QUICK REFERENCE TO PSYCHOTROPIC MEDICATIONS® to see how each drug affects serotonin, norepinephrine, and dopamine.
- Review CYP enzyme interactions: Is the new drug a strong inhibitor of CYP2D6, 2C19, or 3A4? If yes, check what else the patient is taking.
- Assess narrow therapeutic index drugs: Lithium, carbamazepine, clozapine, and valproate need close monitoring. A small change in dose or interaction can push levels into toxicity.
- Implement first-dose monitoring: After starting a new combo, observe the patient for 2-4 hours. Watch for agitation, sweating, confusion, rapid heart rate.
- Set up a follow-up plan: Schedule check-ins at days 3, 7, and 10. Use standardized tools: PHQ-9 for depression, GAD-7 for anxiety, AIMS for movement disorders.
What You Can Do as a Patient
You don’t need to be a pharmacist to protect yourself. Here’s how:- Keep a full list of everything you take: Prescriptions, supplements, herbs, OTC meds-even occasional use. Include dosages and why you take them.
- Ask your doctor: “Could this interact with anything else I’m taking?” Don’t assume they know. Many don’t.
- Use a drug interaction checker: Apps like Epocrates or Medscape are free and reliable. Enter all your meds and see what pops up.
- Never start a new medication without telling your psychiatrist: Even if it’s “just” melatonin or St. John’s wort. St. John’s wort is a serotonin booster-dangerous with SSRIs.
- Know the warning signs of serotonin syndrome: Shivering, diarrhea, fast heart rate, high blood pressure, muscle stiffness, fever, confusion. If you feel this after starting a new med, go to the ER.
New Tools Are Helping-But They’re Not Perfect
Technology is catching up. Digital monitoring tools now alert doctors in real time when a dangerous combo is prescribed. One study showed a 37% drop in serious interactions when these systems were used properly. Pharmacogenomic testing is another big step. Testing for CYP2D6 and CYP2C19 genes can tell you if you’re a slow or fast metabolizer. If you’re a slow metabolizer of SSRIs, even a standard dose could build up to toxic levels. The Clinical Pharmacogenetics Implementation Consortium (CPIC) updated its guidelines in 2022 to guide these decisions. But here’s the catch: most insurance plans still don’t cover these tests. And not all doctors know how to interpret them. So while the science is advancing, access isn’t keeping pace.The Bottom Line
Psychiatric medications are powerful. They can restore your life. But they’re not harmless. When combined, they can turn from healing to hazardous in minutes. The risk isn’t in taking multiple meds-it’s in taking them without understanding how they work together. The solution isn’t to avoid treatment. It’s to treat smarter. Talk to your doctor. Ask questions. Demand a full review of your meds. Use a drug interaction tool. Know the signs of trouble. Your life might depend on it.Can I take melatonin with my antidepressant?
Melatonin is generally safe with most antidepressants, but it can slightly increase serotonin levels. If you’re taking an SSRI or SNRI, start with a low dose (0.5-1 mg) and watch for increased drowsiness or agitation. Avoid high doses (over 5 mg), especially if you’re also on tramadol, linezolid, or MAOIs.
Is it safe to drink alcohol while on psychiatric meds?
No, it’s not safe. Alcohol amplifies sedation from TCAs, antipsychotics, and benzodiazepines. It can worsen depression, increase dizziness, and raise the risk of falls. With MAOIs, alcohol can trigger dangerous blood pressure spikes. Even moderate drinking can interfere with treatment effectiveness and increase side effects.
What should I do if I accidentally take a dangerous combo?
If you suspect a dangerous interaction-especially if you have symptoms like high fever, muscle rigidity, confusion, or rapid heartbeat-call emergency services immediately. Do not wait. Serotonin syndrome and neuroleptic malignant syndrome can escalate quickly. Bring your medication list with you.
How long do I need to wait between stopping an MAOI and starting an SSRI?
Wait at least 14 days after stopping an MAOI before starting an SSRI. For fluoxetine (Prozac), wait 5 weeks because it stays in your system much longer. This washout period is non-negotiable-crossing it can cause serotonin syndrome, which can be fatal.
Are there any antidepressants with the lowest risk of interactions?
Yes. Sertraline and citalopram have fewer enzyme interactions than fluvoxamine or paroxetine. Vilazodone and vortioxetine also have low interaction potential because they don’t strongly inhibit liver enzymes. These are often preferred in patients on multiple medications.
Can herbal supplements interact with psychiatric meds?
Absolutely. St. John’s wort is a major one-it boosts serotonin and can cause serotonin syndrome with SSRIs. Kava can increase sedation with benzodiazepines. Valerian root may enhance effects of antipsychotics. Always tell your doctor about every supplement you take-even if you think it’s “natural.”
Why do some people need blood tests while on psychiatric meds?
Some drugs have a narrow safety margin. Lithium, clozapine, carbamazepine, and valproate can become toxic if levels rise too high. Blood tests ensure you’re getting the right dose. For example, clozapine can cause agranulocytosis-a drop in white blood cells-so weekly blood counts are required for the first 6 months.

Tara Stelluti
This post is literally a horror movie script. I took sertraline and ibuprofen for a headache last week and woke up thinking my bones were turning to glass. I didn't tell anyone. Now I'm scared to breathe.
Abdula'aziz Muhammad Nasir
As a clinical pharmacist in Lagos, I've seen too many patients on SSRIs with St. John’s wort or local herbal teas that spike serotonin. The real issue isn't the drugs-it's the lack of access to pharmacists who understand polypharmacy. Many patients don't even know their meds have names. They just call them 'the blue one' or 'the one for nerves.' Education is the first line of defense.
Margaret Wilson
Oh wowwwww so you're telling me my 5mg melatonin + Lexapro + chamomile tea + CBD gummies = serotonin apocalypse??? 😭 I thought I was just being *self-care queen* 🌿✨ I'm gonna need a therapist to unsee this.
william volcoff
It’s funny how we treat psychiatric meds like they’re vitamins. You wouldn’t mix random painkillers without checking interactions, but we’ll toss three antidepressants and a sleep aid together like it’s a smoothie. The system’s broken, not the patients. And yes, fluoxetine’s 5-week washout? Non-negotiable. I’ve seen the ER reports.
Freddy Lopez
Medication is not a cure-it’s a tool. But we’ve turned it into a crutch, then a sacrament, then a secret. The real danger isn’t serotonin syndrome. It’s the silence around it. We fear asking questions because we’ve been taught to trust authority blindly. But the brain is not a black box. It’s a network. And networks fail when we ignore the connections.
Brad Samuels
I’ve been on lithium for 12 years. Took ibuprofen once for a migraine. Ended up in the ER with tremors and nausea. They didn’t even ask what I was on. I’ve learned to carry a card in my wallet now. If you’re on anything psychiatric, do the same. It saved my life.
Jeff Moeller
Pharmacogenomics is the future but nobody’s talking about the cost. My cousin got tested for CYP2D6. Insurance denied it. So she paid $600 out of pocket. Then her psychiatrist didn’t know how to read the results. The system is designed to fail us. We’re not patients. We’re data points with a side of anxiety.
Herbert Scheffknecht
What if the real danger isn’t the drugs but the belief that we need drugs at all? We’ve pathologized sadness. We’ve medicalized grief. We’ve turned human experience into a chemical imbalance that needs fixing. Maybe we should be asking why we’re so broken instead of what cocktail will numb it. The system doesn’t want you healed. It wants you medicated. Forever.
Jessica Engelhardt
Big Pharma is running the show. They don’t want you knowing about interactions because then you’d stop taking their $1000/month pills. They profit from confusion. They profit from ER visits. They profit from blood tests. They profit from fear. The FDA? Bought and paid for. Read the documents. It’s all there. Wake up.
Danielle Mazur
They’re hiding something. Why is fluoxetine’s half-life so long? Why do they push MAOIs at all? Why is there no public database of all fatal interactions? This isn’t medicine. It’s social engineering. They want us docile. They want us dependent. And they want us quiet. Don’t trust the system. Never trust the system.