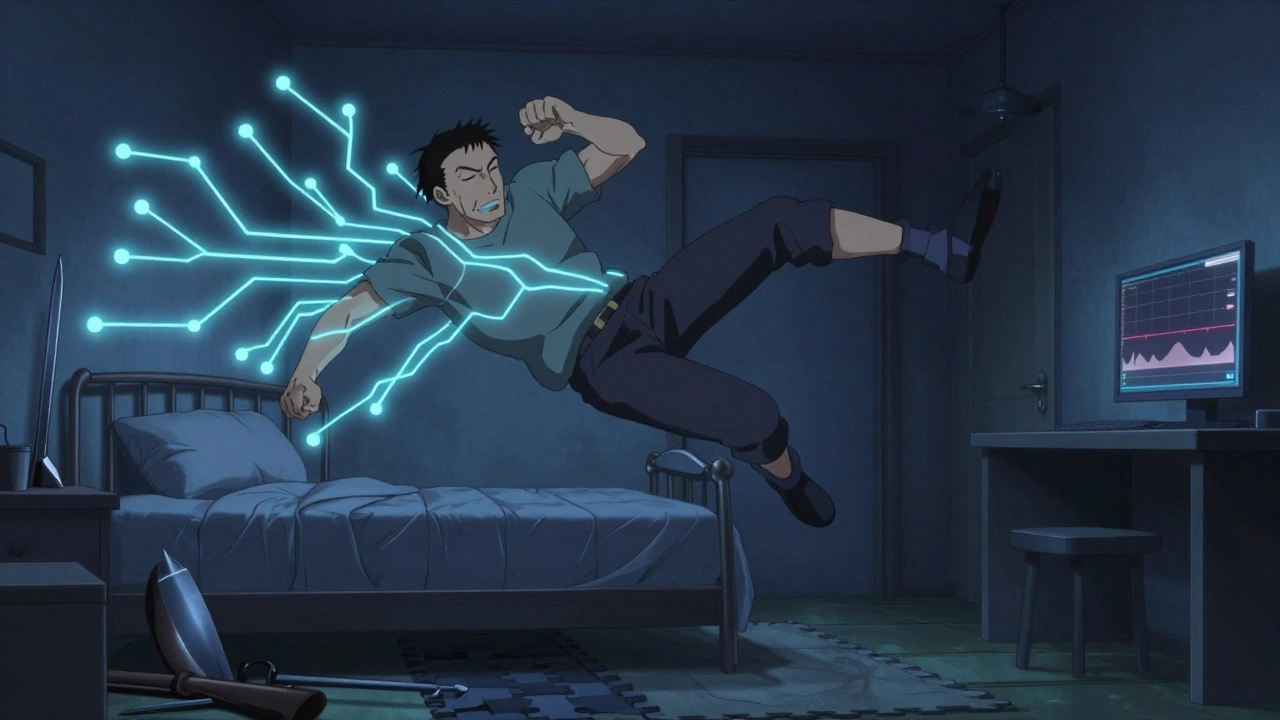
REM sleep behavior disorder isn’t just about acting out dreams. It’s a warning sign your brain is changing - and it could signal something much bigger down the road. People with this condition punch, kick, yell, or even jump out of bed while dreaming, often without remembering it the next morning. Their bodies don’t shut down during REM sleep like they should. Instead, they move. And that movement isn’t harmless. Falls, broken bones, and injuries to bed partners are common. In fact, 78% of people with this disorder make major changes to their bedrooms just to stay safe - removing sharp furniture, installing bed rails, and even locking away weapons.
What makes this more than a sleep problem is what it might mean for your brain. About 90% of people with REM sleep behavior disorder (RBD) will eventually develop a neurodegenerative disease like Parkinson’s, dementia with Lewy bodies, or multiple system atrophy. That’s not a guess. It’s backed by years of tracking. One major study found 73.5% of people with idiopathic RBD developed one of these conditions within 12 years. That’s why seeing a neurologist isn’t optional - it’s essential. This isn’t just about sleeping better. It’s about catching something serious before it’s too late.
How RBD Is Diagnosed: The Role of Polysomnography
You can’t diagnose RBD by asking someone if they dream loudly. You need hard data. That’s where polysomnography (PSG) comes in. This overnight sleep study records brain waves, eye movements, heart rate, breathing, and muscle activity. The key finding? REM sleep without atonia - or RSWA. Normally, during REM sleep, your muscles are paralyzed to stop you from acting out dreams. In RBD, that paralysis fails. The muscles stay active.
The International Classification of Sleep Disorders says RSWA must be present in at least 15% of REM sleep epochs to confirm RBD. In practice, that means technicians look for bursts of muscle activity in the chin, legs, or arms during REM phases. On average, people with RBD show complex movements about 4.2 times per hour. That’s not occasional thrashing - it’s frequent, repeated, and often violent.
Doctors also rule out other causes. Seizures, certain medications, alcohol withdrawal, or other sleep disorders can mimic RBD. A full neurological exam is part of the process. If you’re over 50, have balance issues, or show early signs of tremor or memory problems, that changes the picture. RBD in older adults is rarely isolated. It’s a red flag.
First-Line Treatments: Melatonin vs. Clonazepam
There are no FDA-approved drugs specifically for RBD. But two medications are used off-label as standard care: melatonin and clonazepam. Both work, but they’re very different.
Melatonin is a natural hormone that helps regulate sleep. For RBD, it’s given in doses between 3 mg and 12 mg at bedtime. Studies show about 65% of patients see a big drop in dream enactment. One 68-year-old man went from seven episodes a week to just one after starting 6 mg nightly. Side effects are mild - maybe a bit of morning grogginess, or a headache. Most people tolerate it well. It’s especially good for older adults or those with other health issues because it doesn’t cause dizziness or increase fall risk.
Clonazepam, a benzodiazepine, works faster and stronger. It suppresses muscle activity during sleep. Around 80-90% of people respond to it. In one 2000 study, 88.7% of patients had fewer or no episodes. A spouse reported, “After my husband started 0.5 mg, I could finally sleep in the same bed without fear of being kicked.” But the risks are real. Dizziness affects 22% of users. Unsteadiness hits 18%. Daytime sleepiness is common. For people over 65, the risk of falling increases by 34%. Long-term use can lead to dependence, tolerance, and withdrawal nightmares if stopped suddenly.
Because of this, many neurologists now start with melatonin - especially for older patients. A 2022 survey of 450 neurologists showed 58% choose melatonin first. Only 32% start with clonazepam. Combination therapy is used in about 10% of cases.

Other Medications: What Works and What Doesn’t
Some patients don’t respond to melatonin or clonazepam. Others have side effects they can’t tolerate. That’s when doctors turn to other options.
Pramipexole, a dopamine agonist used for Parkinson’s and restless legs syndrome, helps about 60% of RBD patients. It’s especially useful if someone has both RBD and RLS. Doses are low - 0.125 to 0.5 mg daily. But it can cause nausea, dizziness, or impulse control problems. It’s not a first choice unless other symptoms are present.
Rivastigmine, an Alzheimer’s drug, showed promise in one small trial for patients with RBD and mild cognitive impairment who didn’t respond to standard treatment. It improved dream enactment frequency. But there’s not enough data to recommend it widely.
Dual orexin receptor antagonists are the most exciting new development. Drugs like suvorexant (Belsomra) and NBI-1117568 - still in trials - target the brain’s wakefulness system. Mount Sinai research in October 2023 found these drugs reduced dream enactment behaviors by 78% in animal models. Early human data is promising. The FDA gave Fast Track status to NBI-1117568 in January 2023. If Phase III trials succeed, this could become the first truly targeted RBD treatment - with fewer side effects than clonazepam and more reliable than melatonin.
Safety First: Modifying the Bedroom Environment
No medication works perfectly. Even with treatment, episodes can still happen. That’s why safety changes aren’t optional - they’re life-saving.
The Cleveland Clinic recommends:
- Remove all weapons from the bedroom - guns, knives, tools
- Pad sharp corners of furniture
- Place thick carpets or foam mats next to the bed
- Install bed rails or use a low bed
- Consider sleeping in separate beds if episodes are severe
Even with meds, 42% of patients eventually sleep apart from their partners. That’s not failure - it’s practical. One study found that 78% of families made at least three safety changes. Many don’t realize how dangerous this can be until someone gets hurt.
Also, avoid alcohol. Even one or two drinks can trigger an episode in 65% of people with RBD. It doesn’t matter if you drink at dinner or before bed - it disrupts the brain’s ability to maintain muscle paralysis during REM sleep.
Neurological Monitoring: Watching for the Next Step
Because RBD often precedes Parkinson’s or dementia, regular neurological checkups are critical. The American Academy of Neurology recommends annual evaluations for anyone diagnosed with idiopathic RBD.
What are doctors looking for? Early signs of movement disorders: slight tremor, reduced arm swing while walking, stiffness, or changes in smell or constipation. Cognitive changes like trouble remembering names, getting lost in familiar places, or losing interest in hobbies are also red flags.
The conversion rate is about 6.3% per year. That means over 10 years, most people with RBD will develop a neurodegenerative disease. But catching it early changes everything. Parkinson’s treatments work best when started before symptoms become severe. Dementia interventions can slow decline if started in the mild stage.
This is why RBD is now seen as a prodromal marker - an early signal of brain change. Researchers are even using RBD as a way to test new drugs that might delay or prevent Parkinson’s. Clinical trials are underway to see if early treatment with neuroprotective agents can stop the disease before it fully develops.
What’s Next: The Future of RBD Treatment
The field is changing fast. The global RBD market is worth $1.2 billion and growing at 5.7% a year. Why? Because awareness is rising. More sleep centers are testing for RSWA. More neurologists are connecting RBD to neurodegeneration.
But the real breakthrough will come when we move from symptom control to disease modification. Right now, we treat the dreams - not the brain degeneration behind them. The next five years could bring the first therapies that slow or stop Parkinson’s in people with RBD.
Dr. Ronald Postuma from McGill University says it plainly: “The next five years will likely see the first disease-modifying therapies targeting the underlying neurodegenerative process in RBD patients.” That’s the holy grail.
Until then, the best approach is simple: diagnose early, treat symptoms safely, make the bedroom secure, and monitor the brain closely. Melatonin and clonazepam aren’t perfect - but they work. And they buy time. Time to prepare, time to plan, and maybe, one day, time to prevent what’s coming next.
Hamza Laassili
So let me get this straight... you're telling me if I start kickin' my wife in the sleep, I'm basically signing up for Parkinson's?? Jesus Christ. I thought I was just a restless sleeper. Now I'm gonna need to buy a mattress with bulletproof padding and a gun safe. #RBDisreal
Rawlson King
The data is clear. REM sleep behavior disorder is not a sleep disorder. It is a neurodegenerative prodrome. The clinical implications are profound. Ignoring it is medically indefensible. The 90% conversion rate is not speculative. It is longitudinal and replicated. This is not a suggestion. It is a mandate for neurological evaluation.
Constantine Vigderman
Guys I just found out my dad has this and I'm so glad I read this!! He was always yelling in his sleep and I thought he was just having bad dreams. Now I get why he keeps a foam pad under his bed and why he won't let me near his toolbox 😅. Melatonin seems way safer than clonazepam for him-he's 72 and already trips over air. Let's spread the word!! This could save lives!! 🙌
Cole Newman
You people are overreacting. I’ve been acting out my dreams since I was 19. I’ve never had Parkinson’s. My wife says I yell about dinosaurs sometimes. That’s not a disease, that’s a personality. You’re all scared of your own shadow. Also, melatonin? That’s just a fancy vitamin. If you want results, take something real. Like a shot of whiskey. Works every time.
Casey Mellish
As an Australian, I’ve seen this play out in my uncle’s case. He was diagnosed with idiopathic RBD at 64. Five years later, he got diagnosed with Lewy body dementia. The thing nobody talks about? The emotional toll on families. My aunt had to move into a separate room. She stopped sleeping. He stopped recognizing her. The meds help with the kicking, but they don’t fix the loneliness. This isn’t just about brain chemistry. It’s about human connection.
Tyrone Marshall
There’s a quiet dignity in facing this head-on. You don’t need to be a neuroscientist to understand the gravity: your body is betraying you before your mind even knows. The fact that we can intervene early-before tremors, before memory loss-is a gift. Not everyone gets that warning. RBD gives us time. Time to say what needs to be said. Time to rearrange the furniture. Time to hold someone’s hand before the lights go dim. That’s not medical jargon. That’s life.
Emily Haworth
Wait… so if you have RBD, you’re basically a walking time bomb for Big Pharma? 🤔 I mean, who benefits? The sleep labs? The drug companies? The neurologists? I’m not saying it’s fake, but why is this only being studied NOW? And why are they pushing melatonin like it’s magic? I’ve seen ads for suvorexant everywhere. Coincidence? Or is this a stealthy way to sell us expensive drugs before we even get sick? 🚨 #RBDconspiracy
Tom Zerkoff
The clinical guidelines are unequivocal. Polysomnographic confirmation of REM sleep without atonia, in conjunction with a comprehensive neurological assessment, constitutes the diagnostic standard. The efficacy of melatonin as a first-line agent is supported by multiple randomized controlled trials. The risk-benefit profile of clonazepam, particularly in the geriatric population, necessitates caution. Further, environmental modifications are not adjunctive-they are integral to patient safety. This is not a matter of opinion. It is evidence-based medicine.
Yatendra S
I think this is like… the universe giving you a dream before the real nightmare begins. Like your soul is trying to warn you. Maybe it’s karma. Maybe it’s the soul leaving before the body. I don’t know. But I feel like if you act out your dreams… maybe you’re already half-dead inside. And the rest is just waiting for the body to catch up. 🤔🕯️
Himmat Singh
The assertion that 90% of RBD patients will develop neurodegenerative disease is statistically misleading. The cohort studied was highly selected-predominantly elderly males with comorbidities. Generalization to the broader population is invalid. Furthermore, the definition of idiopathic RBD lacks standardization across institutions. The data is not as robust as claimed. Caution is warranted before pathologizing normal dream enactment.
kevin moranga
I just want to say-this post saved my marriage. My wife used to sleep on the couch because I’d punch the air like I was fighting a ghost. We thought it was stress. Turns out, I had RBD. Started melatonin at 6mg, padded the corners, got rid of my knife collection (yes, I had a knife collection… don’t ask). Now we sleep in the same bed again. I still yell about space whales sometimes, but she says it’s kinda cute. Seriously, if you or someone you love is doing this-don’t ignore it. Don’t wait. Do the things. Change the room. Take the pill. It’s not weakness. It’s love in action. ❤️