When you’re taking blood pressure medication, every bite of food matters more than you think. That bag of chips, the canned soup, even the bread you grab for breakfast - they’re not just snacks or staples. They’re quiet saboteurs of your treatment. If you’re eating too much salt, your pills might as well be half-empty.
Why Salt Makes Your Blood Pressure Meds Work Less
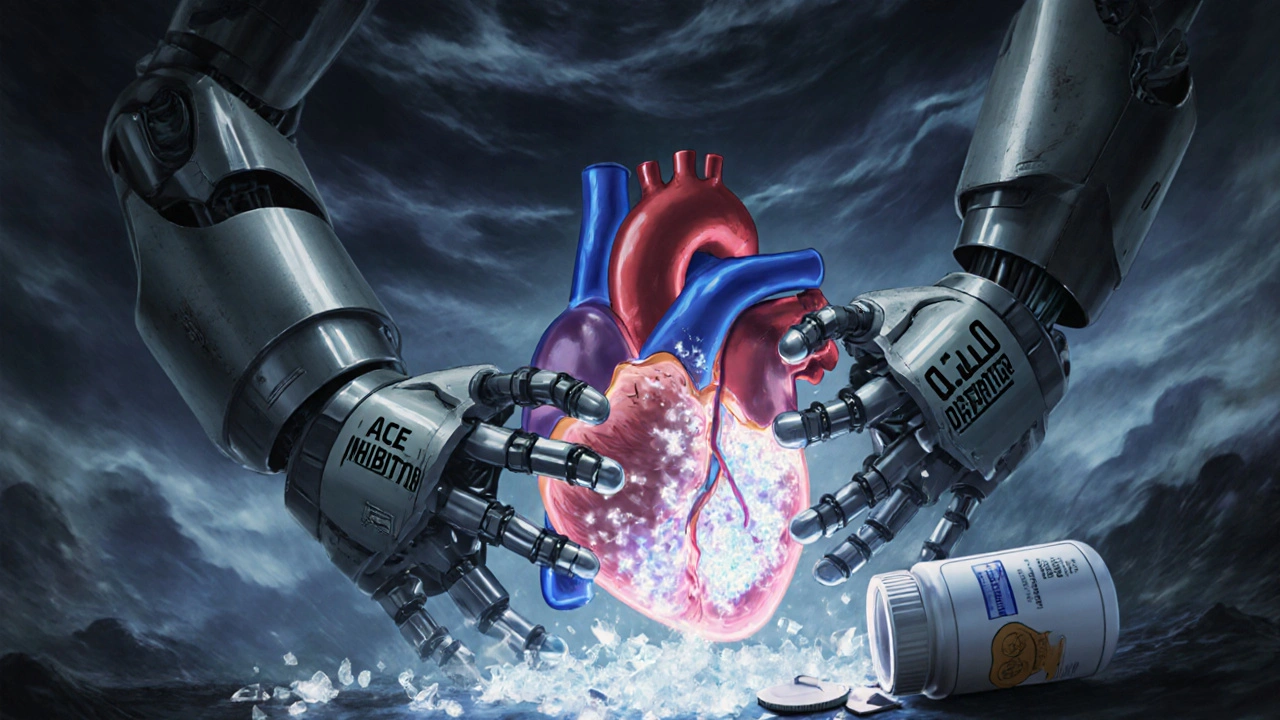
Your body doesn’t handle sodium like a simple seasoning. Too much of it floods your bloodstream, pulling water into your blood vessels and forcing your heart to pump harder. That’s what raises your blood pressure. Now, imagine you’re taking an ACE inhibitor or a diuretic to lower it. These drugs work by relaxing blood vessels or flushing out extra fluid. But if you keep dumping in sodium, your body fights back - it holds onto water, your vessels stay tight, and the meds lose their punch. A major 2023 study published in JAMA tracked 213 adults on blood pressure medication. When they cut sodium by about one teaspoon a day (2,300 mg), their systolic blood pressure dropped by 6 mm Hg. That’s the same drop you’d expect from starting a new pill. And here’s the kicker: it happened in just one week. No new drugs. No extra visits. Just less salt.Who’s Most Affected? You Might Be Surprised
Not everyone responds the same way to sodium. About 25-30% of people are what doctors call “salt-resistant” - their blood pressure barely budges when they cut back. But that doesn’t mean the advice doesn’t apply to them. The other 70-75%? They see real results. And the people who benefit the most are often the ones you’d least expect. Older adults, Black individuals, and those with diabetes or kidney disease show the strongest drops in blood pressure when sodium is lowered. In fact, hypertensive patients saw nearly double the benefit of those with normal blood pressure. A 100 mmol drop in daily sodium (roughly 2,300 mg) led to a 5.4 mm Hg systolic drop in people with high blood pressure - compared to just 2.4 mm Hg in those without. If you’re over 50, have a family history of hypertension, or are on medication already, you’re likely in the group that needs this change the most.Where the Salt Is Hiding (It’s Not in Your Shaker)
Most people think they’re cutting salt by skipping the salt shaker. That’s like trying to lose weight by avoiding sugar in your coffee while still eating donuts. About 70% of the sodium we consume comes from packaged, processed, and restaurant foods. Think: frozen meals, deli meats, soy sauce, salad dressings, canned beans, bread, and even sweet stuff like cereal and granola bars. Here’s what to look for on labels: anything with more than 140 mg of sodium per serving is high. If a product says “low sodium,” check the actual milligrams - some brands slap that label on things with 200 mg per serving. That’s still too much if you’re trying to get under 1,500 mg daily. And don’t be fooled by “no added salt” claims. That doesn’t mean low sodium. Canned tomatoes, for example, often have sodium naturally present or added during processing. Always read the nutrition facts - not the front-of-package marketing.How Much Salt Is Too Much? The Numbers That Matter
The American Heart Association says the ideal daily limit is 1,500 mg. That’s less than two-thirds of a teaspoon. The absolute maximum? 2,300 mg - still less than one teaspoon. But most people in the U.S. and Australia eat between 3,000 and 4,500 mg a day. That’s double or even triple what’s recommended. In the JAMA study, participants’ usual diets averaged 4,500 mg daily. When they dropped to 500 mg total sodium (not added - total), their systolic pressure fell to 119 mm Hg. That’s a drop of 7-8 mm Hg from their high-sodium days. And they didn’t feel worse. No dizziness. No fatigue. Just better numbers. Even cutting from 4,500 mg to 3,000 mg helped. You don’t need to go from zero to hero overnight. Start by reducing by 1,000 mg a day. That’s often enough to feel a difference in how your meds work.
Which Medications Are Most Impacted?
Not all blood pressure drugs are equally affected by sodium. But the ones that rely on reducing fluid volume or relaxing blood vessels take the biggest hit:- Diuretics (like hydrochlorothiazide) - they flush out fluid, but excess sodium makes your body hold onto water again.
- ACE inhibitors (like lisinopril) and ARBs (like losartan) - they relax blood vessels, but sodium keeps them tense.
- Calcium channel blockers - less affected, but still benefit from lower sodium.
- Beta-blockers - minimal direct interaction, but overall blood pressure control improves with less salt.
What About Salt Substitutes? Are They Safe?
Potassium chloride salt substitutes can help reduce sodium without losing flavor. But they’re not for everyone. If you have kidney disease, take certain blood pressure meds (like ACE inhibitors or ARBs), or have high potassium levels, these substitutes can be dangerous. Too much potassium can cause heart rhythm problems. Before you swap your salt, talk to your doctor. Get a blood test to check your potassium. If your kidneys are healthy and you’re not on meds that raise potassium, a salt substitute can be a smart tool. But if you’re unsure, skip it. There are plenty of other ways to flavor food: herbs, garlic, lemon, vinegar, smoked paprika, cumin - all work wonders.How to Start Cutting Salt - A Realistic Plan
You don’t need to overhaul your life overnight. Start here:- Check one meal a day. Pick breakfast. Swap sugary cereal for plain oats with fruit. Replace bacon with grilled chicken or eggs. Read labels - even one change can cut 500 mg.
- Use herbs and spices. Keep a spice rack. Try turmeric, rosemary, black pepper, chili flakes. They add flavor without sodium.
- Choose fresh or frozen without sauce. Frozen veggies without butter or salt, fresh chicken, plain rice - these are your allies.
- Don’t add salt at the table. Give your taste buds a week to adjust. You’ll start noticing other flavors.
- Track your sodium for 3 days. Use a free app like MyFitnessPal. You’ll be shocked how fast it adds up.

The Bigger Picture: It’s Not Just About Pressure
Lowering salt doesn’t just help your blood pressure numbers. It protects your kidneys. High sodium increases protein in your urine - a sign your kidneys are under stress. That’s especially bad if you have diabetes. Medications like ACE inhibitors help reduce that protein, but only if you’re not drowning in salt. It also helps your heart. Less sodium means less strain on your arteries, lower risk of stroke, and less chance of heart failure. The American Heart Association estimates that if everyone cut sodium to 2,000 mg a day, we could prevent 280,000 to 500,000 heart-related deaths over ten years. And here’s the quiet win: when sodium drops, your body starts to feel better. Less bloating. Less puffiness. Better sleep. More energy. These aren’t side effects - they’re signs your system is finally working the way it should.What If You Don’t See Results?
If you’ve cut salt for 4-6 weeks and your blood pressure hasn’t changed, don’t give up. You might be in the 25-30% who are less sensitive. But that doesn’t mean it’s pointless. You still reduce your risk of kidney damage, heart rhythm issues, and stroke. And sometimes, the benefit shows up slowly - or in how you feel, not just in the numbers. Talk to your doctor. Ask if you should check your potassium, test for kidney function, or consider a 24-hour urine sodium test. Some clinics now offer personalized sodium targets based on your meds and health history.Final Thought: Your Pills Are Only Half the Story
Taking your blood pressure medication is important. But if you’re still eating like you’re on a road trip with no access to fresh food, you’re fighting a losing battle. Salt doesn’t just add flavor - it adds pressure. And that pressure makes your meds work harder, or worse, useless. You don’t need to become a nutritionist. You don’t need to eat bland food. You just need to be aware. Read labels. Cook more. Choose fresh. Cut the processed stuff. And give your body a chance to respond. The science is clear: less salt = better results. Your pills are ready. Are you?Can I still eat out if I’m trying to reduce sodium for my blood pressure meds?
Yes, but you need to be strategic. Skip the soups, sauces, and dressings. Ask for meals to be prepared without added salt. Choose grilled or steamed proteins, plain rice or potatoes, and steamed vegetables. Chains like Chipotle and Panera allow you to customize - select "no salt" on the app or ask the staff. Avoid fried items and anything labeled "seasoned," "marinated," or "crispy." Even a simple grilled chicken salad with oil and vinegar can be low-sodium if you skip the croutons and bottled dressing.
How long does it take to see a difference in blood pressure after cutting salt?
Many people see a drop in blood pressure within 3-7 days. In the 2023 JAMA study, participants showed measurable changes after just one week of low-sodium eating. The biggest drops usually happen in the first two weeks. But for some, especially those with long-term high sodium intake, it may take 4-6 weeks to see the full effect. Consistency matters more than perfection.
Does cutting salt mean I can stop taking my blood pressure medication?
No. Never stop or reduce your medication without talking to your doctor. While cutting salt can improve how well your meds work - and sometimes even allow for a lower dose - it doesn’t replace them. Blood pressure medication treats the condition; reducing sodium supports the treatment. Think of it like exercise and insulin for diabetes: one helps the other, but you still need both.
Are there side effects to eating less salt?
For most people, there are no harmful side effects. Some report mild fatigue or headaches in the first few days as their body adjusts, but these usually pass. In rare cases, people with certain conditions (like Addison’s disease or severe heart failure) may need to monitor sodium more carefully - but this is uncommon. The real risk isn’t too little salt - it’s too much. The average person eats 2-3 times the recommended amount, which is far more dangerous than going slightly below.
What’s the best way to track my daily sodium intake?
Use a free app like MyFitnessPal or Cronometer. Scan barcodes or search foods by name. Focus on the actual milligrams (mg) of sodium, not the % Daily Value. A good rule: if a food has more than 140 mg per serving, it’s high. Aim to keep your total under 1,500 mg daily. Keep a simple notebook if you prefer - write down everything you eat and look up the sodium content online. After a few days, you’ll start recognizing which foods are sneaky.
Geethu E
OMG I had no idea my canned beans were sabotaging my meds! I switched to rinsing them and my BP dropped 8 points in 10 days. My doctor was shocked. Also, skip the soy sauce-use coconut aminos. Game changer.
anant ram
Listen: salt isn't the enemy-processed food is. You don't need to be a monk. Just stop eating anything that comes in a box with a barcode longer than your thumb. I did this. Lost 12 lbs. BP normal. No new pills. Just real food.
king tekken 6
Okay but like… what if sodium is just a distraction? Like… what if the real issue is corporate greed? Big Pharma wants you on meds. Big Food wants you addicted to salt. It’s all connected. We’re being played. I mean… think about it. Why else would the AHA push 1500mg? It’s not science-it’s control. 🤔
DIVYA YADAV
India has been eating low-sodium diets for centuries-tadka, curry leaves, asafoetida, lime, ginger-no salt needed. But now we’re copying American junk food and wondering why our parents are dying of hypertension. This isn’t a medical issue-it’s cultural betrayal. Our grandparents didn’t need pills. They had taste. We have flavorless, sodium-soaked plastic. Wake up.
Kim Clapper
I find it deeply concerning that this article implies personal responsibility is sufficient to manage systemic health outcomes. One cannot reasonably expect individuals to navigate a labyrinth of deceptive labeling, subsidized processed foods, and aggressive marketing campaigns while simultaneously managing chronic illness. This is not empowerment-it is victim-blaming disguised as advice.
Bruce Hennen
Diuretics and ACE inhibitors are absolutely compromised by sodium. The mechanism is well-documented. But calcium channel blockers? They work independently of volume status. So if your BP isn’t budging, check your meds-not just your salt. You might be on the wrong class. Also, 1500mg is a myth. WHO says 2000mg is fine for most. Don’t become orthorexic.
Jake Ruhl
so like… i tried cutting salt and i felt like a zombie for 3 days. then i started eating more avocado and bananas and my energy came back. but then i saw a video on tiktok that said potassium is bad if you have kidney issues and now i dont know if im saving my heart or killing my kidneys. help. also my cat licked my salt substitute and i think she’s mad at me.
Chuckie Parker
USA has the worst food system on earth. Every single processed item is engineered to be addictive. They don't care if you die. They care about profit. Stop blaming yourself. The system is rigged. Fight the corporations not your cravings.
Michael Segbawu
my mom took her meds and ate chips every day for 10 years. her BP was 180/110. she cut salt. went to 120/78. no new pills. just stopped eating the crap. she’s 72 and walks 5 miles a day. if she can do it you can too. stop making excuses.
Aarti Ray
i cook indian food at home and never use salt. just cumin, turmeric, green chilies, and lemon. my husband thought i was crazy but his bp dropped 10 points. now he adds garlic powder and says it tastes better. we still eat out but ask for no salt. they always say yes. you just have to ask
Alexander Rolsen
Let’s be real: the only reason this works is because people who care enough to read this article are already the ones who are motivated. The people who need it most? They’re eating microwave dinners while scrolling on their phones. No amount of advice will reach them. The system is broken. We’re just rearranging deck chairs.
Leah Doyle
thank you for this!! i started tracking my sodium and i had no idea how much was in my "healthy" granola bar-320mg!! now i make my own with oats and dates. also i started using smoked paprika and it’s like magic. i feel less bloated and my skin looks better. i didn’t even know that was a thing 😊
Alexis Mendoza
It’s funny how we think medicine fixes things, but the real fix is just… not poisoning ourselves. Salt isn’t evil. But when it’s hiding in everything we eat, it becomes a slow violence. We don’t need more pills. We need more awareness. And maybe, just maybe, less food that looks like plastic.
Geethu E
Replying to Aarti Ray: I do the same! My mom makes dal with just mustard seeds and curry leaves. No salt. We use kokum for sourness. It’s wild how much flavor you can get without sodium. I wish more people knew this.