When a drug company launches a new medicine, the first patent they file protects the active ingredient-the actual chemical that treats the disease. That patent lasts 20 years. But by the time the drug hits the market, five or six of those years are already gone from testing and approval. That leaves maybe 14 years to make back the billions spent on development. So what happens when that clock is ticking down? Companies don’t just wait. They file secondary patents.
What Exactly Are Secondary Patents?
Secondary patents aren’t about the drug’s core chemistry. They’re about everything else: how it’s made, how it’s taken, what form it’s in, or even what new disease it can treat. These patents cover things like:- A new crystal form of the drug (called a polymorph)
- A special coating that makes it release slowly over 12 hours
- A different salt version that’s easier to absorb
- A new use-for example, turning a sleep aid into a treatment for multiple myeloma
- A combination of two drugs in one pill
These aren’t always groundbreaking science. Some are small tweaks. But under patent law, if they’re novel and non-obvious, they get protection. And that protection can add years-sometimes a decade-to how long a drug stays off-limits to generics.
How They Delay Generic Drugs
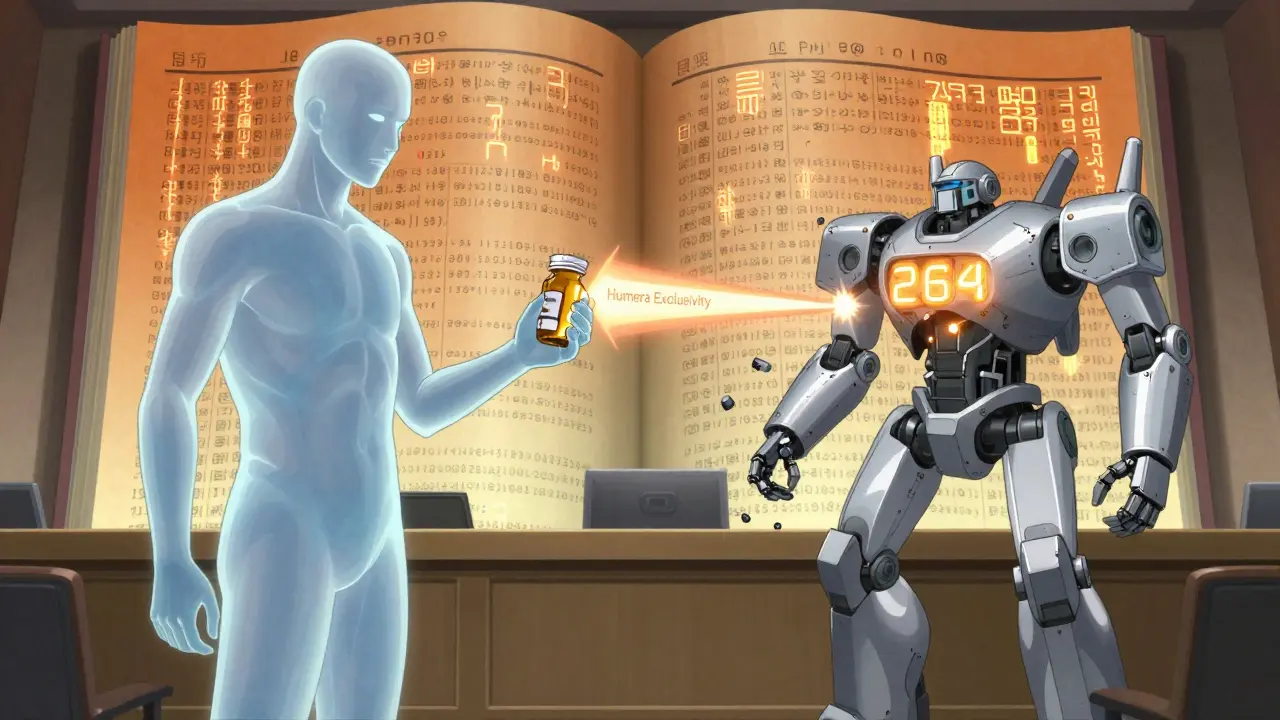
The U.S. Food and Drug Administration keeps a public list called the Orange Book. It only includes certain types of patents: formulation, method of use, and some compound patents. When a generic company wants to sell a cheaper version, they must check this list. If they see a patent, they can either wait-or challenge it in court.Here’s where it gets strategic. A single drug can have dozens of secondary patents. Humira, for example, had 264 of them. Even though the main patent expired in 2016, generic versions couldn’t enter until 2023. Why? Because every time one patent was challenged, another one kicked in. It’s called a patent thicket-a dense, tangled web of overlapping protections that makes it too expensive and risky for generics to enter.
Studies show drugs with secondary patents face generic entry delays that are 2.3 years longer on average than those without. And for blockbuster drugs earning over $1 billion a year, it’s common to have 10 or more secondary patents. Pfizer alone held over 14,000 active secondary patents as of 2023.
Real-World Examples That Changed the Game
One of the most famous cases is AstraZeneca’s Nexium. Before Nexium, there was Prilosec, a popular heartburn drug. Prilosec’s patent was set to expire. But AstraZeneca had already developed its single-enantiomer version-just one mirror-image molecule of the original compound. That version, Nexium, was marketed as more effective and safer. It wasn’t dramatically better, but it was enough to get a new patent. Nexium became a $5 billion-a-year drug, extending exclusivity for nearly 8 years.Another example is GlaxoSmithKline’s Paxil. The original patent on paroxetine expired in 2001. But a specific crystalline form-Form G-was patented later. That patent blocked generics until 2005. Patients didn’t notice a difference. Doctors didn’t see improved outcomes. But the company kept its monopoly.
Even drugs with bad reputations got second lives. Thalidomide, once linked to birth defects, was re-patented in the 1990s for treating leprosy, then again in 2006 for multiple myeloma. Each new use got a new patent. Each one pushed back the day generics could come in.
The Cost to Patients and the System
The result? Higher prices. When a drug has no competition, companies can charge whatever they want. Humira cost $20 billion a year in U.S. spending before generics arrived. That’s money paid by insurers, Medicare, and patients. Pharmacy benefit managers like Express Scripts say secondary patents raise their costs by 8.3% every year.Doctors report confusion too. Patients come in asking if they should switch from the old generic to the new branded version-even though the active ingredient is the same. Pharmaceutical reps push the newer version right before generics hit the market. It’s called product hopping. And it works.
For generic manufacturers, the legal fight is brutal. It costs $15-20 million to challenge a single secondary patent. And even if they win, the process can take years. In 2022, generics filed challenges against 92% of listed secondary patents-but only 38% succeeded in court.
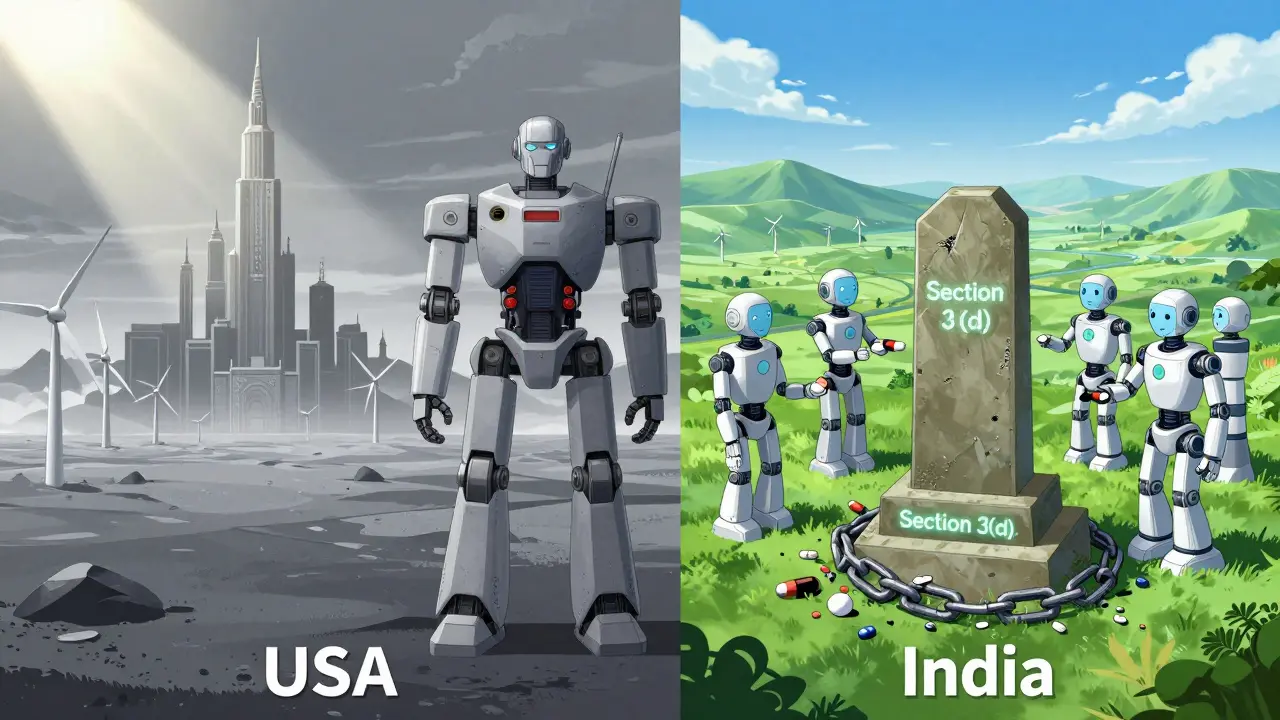
Global Differences: Where It’s Stopped
Not every country plays by the same rules. India’s patent law, since 2005, has a clause called Section 3(d). It says you can’t patent a new version of an existing drug unless it shows a significant improvement in effectiveness. That’s why Novartis lost its bid to patent a modified version of Gleevec. The Indian court said the new form wasn’t better-just different. That decision opened the door for affordable generics across the developing world.Brazil requires extra approval from its health ministry before granting pharmaceutical patents. The European Union asks for proof of “significant clinical benefit” before allowing certain secondary patents. The U.S. doesn’t require that. That’s why the same drug can be blocked from generics in America while being sold cheaply in India.
Who Supports It-and Who Doesn’t
The pharmaceutical industry defends secondary patents as innovation. PhRMA, the industry’s main lobby, says these patents lead to better dosing, fewer side effects, and new treatments for rare diseases. They point to studies showing secondary patents contribute $14.7 billion annually to R&D funding.But critics call it evergreening-a tactic to keep prices high without real medical progress. Dr. Aaron Kesselheim from Harvard studied over 1,000 secondary patents and found only 12% led to meaningful clinical improvements. The rest? Minor changes that didn’t help patients-but kept profits high.
The UN Development Programme says many secondary patents are “inherently routine.” They argue that if a change doesn’t improve safety or effectiveness, it shouldn’t get 20 years of monopoly protection. The World Health Organization now lists secondary patents as the biggest legal barrier to affordable medicines in 68 low- and middle-income countries.
What’s Changing Now?
Pressure is building. The 2022 Inflation Reduction Act in the U.S. gave Medicare the power to challenge some secondary patents. The European Commission is targeting patent thickets in its new pharmaceutical strategy. Courts are getting stricter too. In 2023, a federal appeals court narrowed how broad antibody patents can be-something that could affect future secondary filings.Analysts predict that by 2027, companies will need to prove their secondary patents offer real patient benefits-not just legal loopholes-to keep public and regulatory support. The days of filing 50 patents on one drug just to delay generics might be ending.
What This Means for You
If you take a brand-name drug and wonder why it’s so expensive, secondary patents are part of the answer. If you’ve been told to switch to a new version of your medication right before the generic arrives, that’s product hopping. And if you live in a country where your medicine is still unaffordable, chances are secondary patents are blocking cheaper options.It’s not about whether innovation matters. It’s about what kind of innovation gets rewarded. Is it the kind that makes a drug safer? Or the kind that just keeps the price tag high?
The system is changing. But for now, secondary patents remain one of the most powerful tools in pharmaceutical business strategy-used not to cure more diseases, but to protect profits for as long as the law allows.
Are secondary patents the same as primary patents?
No. Primary patents protect the active ingredient-the actual chemical compound that treats the disease. Secondary patents protect modifications: how the drug is formulated, how it’s taken, or new medical uses. Primary patents last 20 years from filing. Secondary patents can be filed years later and extend exclusivity beyond that.
Why do generic drug makers struggle to enter the market?
Because brand-name companies file dozens of secondary patents, creating a legal maze called a patent thicket. Generic manufacturers must challenge each patent individually, which costs $15-20 million per drug and can take years. Even if they win one case, another patent may still block entry. Only 38% of legal challenges succeed.
Do secondary patents improve patient outcomes?
Sometimes. About 12% of secondary patents lead to real clinical benefits-like fewer side effects or easier dosing. But most don’t. Studies show many are minor changes-like switching from a tablet to a capsule-that don’t improve health. Yet they still delay cheaper generics for years.
Can countries stop secondary patents?
Yes. India’s patent law (Section 3(d)) blocks patents on new forms of known drugs unless they show significantly improved efficacy. Brazil and the EU also require proof of clinical benefit. These rules help lower drug prices. The U.S. has no such requirement, which is why it has far more secondary patents than other countries.
What is product hopping?
Product hopping is when a drug company releases a slightly modified version of a drug-like a new pill form or extended-release version-just before the original patent expires. They then push doctors and patients to switch, making the old version seem outdated. This delays generic competition because the new version has its own patent.
How many secondary patents can one drug have?
Some drugs have over 100. Humira had 264. The average blockbuster drug has 10-20 secondary patents. Drug Patent Watch found that 89% of drugs earning over $1 billion a year have at least 10 secondary patents. This creates a legal fortress that makes it nearly impossible for generics to enter without a long, costly court battle.
Is there a limit to how long a drug can be protected?
Legally, no. The 20-year patent term applies only to the primary patent. Secondary patents can be filed years after the original, sometimes even after FDA approval. As long as each one meets patent office standards (which vary by country), they can stack up. Some drugs have had exclusivity for over 30 years thanks to layered patents.
What’s next for secondary patents?
Regulators and courts are starting to push back. The U.S. Inflation Reduction Act lets Medicare challenge some secondary patents. The EU and WHO are targeting patent thickets. Experts predict companies will need to prove real clinical benefits to keep winning patent cases. The era of filing patents for trivial changes may be ending-but not yet.
Jason Silva
Bro, this is just Big Pharma’s way of rigging the game 😤💸 They don’t care if you live or die-just that you keep buying their overpriced pills. 264 patents on ONE drug?! That’s not innovation, that’s corporate terrorism. 🤖💊 #WakeUpSheeple
Christina Weber
The term 'secondary patents' is misleading; they are not patents on secondary innovations, but rather on trivial modifications designed solely to extend monopolies. The U.S. Patent and Trademark Office routinely grants these under excessively permissive standards, violating the constitutional mandate to promote 'useful arts.'
Erika Putri Aldana
so like... they just change the color of the pill and call it a new drug? 🤡 why are we still paying $2000 for this? it's literally the same chemical. i'm so done with this system.
Meina Taiwo
In Nigeria, we rely on Indian generics because U.S. secondary patents make drugs unaffordable. This system harms patients globally-not just in America.
Adrian Thompson
This is what happens when the government lets the globalists run the show. Pharma owns the FDA, the courts, and Congress. You think this is coincidence? Nah. It’s a well-oiled machine. And you’re all just pawns. 🇺🇸⚔️
Southern NH Pagan Pride
they call it innovation but its just legal loophole exploitation. the patent office is basically a corporate slush fund. they dont even check if its better for patients. just if the paperwork is right. smh.
Orlando Marquez Jr
The phenomenon described herein constitutes a systemic distortion of the intellectual property regime, wherein economic incentives supplant therapeutic imperatives. The resultant market distortions impose significant burdens upon public health infrastructures, particularly in resource-constrained jurisdictions.
Jackie Be
I CANT BELIEVE WE LET THEM GET AWAY WITH THIS 😭💸 I WAS JUST TOLD TO SWITCH TO A NEW FORM OF MY MEDS AND NOW I’M PAYING 3X MORE AND IT DOES THE SAME THING. THEY’RE LYING TO US AND WE’RE STILL BUYING IT
John Hay
I get why companies do this. They need to recoup R&D costs. But the scale here is insane. We need a better balance-maybe cap the number of secondary patents per drug or require real clinical data. Not just legal tricks.
Jon Paramore
The patent thicket strategy is a textbook example of rent-seeking behavior. By layering non-innovative IP protections, firms internalize downstream monopoly rents. The marginal cost of filing a secondary patent is negligible compared to the $1B+ annual revenue it secures. Regulatory reform must target the 'non-obviousness' standard.
Swapneel Mehta
India’s Section 3(d) is the real hero here. If more countries adopted that, we could save millions. It’s not anti-innovation-it’s pro-patient. Hope the U.S. wakes up before more lives are lost to profit-driven delays.