Blood Thinner Vaccination Safety Checker
Check if you're following CDC guidelines for vaccination while on blood thinners. This tool helps you verify proper techniques to minimize bruising and bleeding risk.
Getting a vaccine while on blood thinners doesn’t mean you have to skip it. But if you’ve ever walked away from a shot with a big, painful bruise, you know why people worry. The good news? With the right technique, you can get vaccinated safely-without ending up with a swollen arm or a trip to the ER.
Why Blood Thinners Make Vaccinations Riskier
Blood thinners like warfarin, Eliquis, Xarelto, and heparin stop clots from forming. That’s lifesaving for people with atrial fibrillation, deep vein clots, or artificial heart valves. But it also means your blood takes longer to stop flowing after a needle puncture. When a vaccine is injected into muscle-like the deltoid in your upper arm-it can cause bleeding under the skin. That’s what leads to hematomas: large, tender bruises that can last for days or even weeks.It’s not common, but it’s real. About 1.2% of people on anticoagulants report serious injection site bleeding after vaccines, according to CDC data from 2022. And while most cases are mild, some patients end up with hematomas so big they limit arm movement. The worst part? Many of these cases happen because the provider didn’t adjust their technique.
What Vaccines Are Safe?
All vaccines currently approved in the U.S. and Australia-including flu shots, pneumococcal, COVID-19 boosters, and shingles vaccines-are safe for people on blood thinners. There’s no vaccine you need to avoid just because you’re on anticoagulants. The CDC, the American College of Chest Physicians, and the Anticoagulation Forum all agree: the risk of catching the flu, pneumonia, or COVID-19 is far greater than the risk of a bruise.Some people worry about the flu shot triggering a spike in INR (a blood test for warfarin users). There are rare case reports of INR rising after vaccination, especially with warfarin. But these are isolated incidents. No such link has been found with newer drugs like Eliquis or Xarelto. If you’re on warfarin, check your INR a day or two before your shot. If it’s under 4.0, you’re good to go. If it’s higher, talk to your doctor about rescheduling.
The Right Needle and the Right Technique
This is where most mistakes happen. Too many clinics still use a 21-gauge needle-thick and blunt-like they’re drawing blood. That’s a recipe for bleeding. The CDC and Anticoagulation Forum recommend a 23-gauge or smaller needle for intramuscular vaccines in people on blood thinners. Smaller needles cause less tissue damage and reduce bleeding risk.Here’s what works:
- Use a 23-gauge or 25-gauge needle. If your provider says they only have 21s, ask them to order the right size. It’s standard practice.
- Inject into the deltoid muscle, not the thigh. The arm has better muscle mass and less risk of hitting major vessels.
- Don’t aspirate (pull back on the plunger). This was once standard to check for blood vessels, but it’s no longer recommended for vaccines-it just adds pain and doesn’t prevent bleeding.
- Apply firm, direct pressure for at least 10 minutes after the shot. No rubbing. No quick pats. Press straight down with your fingers or a gauze pad. If you’re on warfarin or have a history of heavy bruising, ask for 10 minutes. For DOACs like Xarelto or Eliquis, 5 minutes is usually enough.
One patient on Reddit shared: “My nurse used a 25-gauge needle and held pressure for 10 minutes. Zero bruising. My last shot? 21-gauge, 30-second press. I had a golf ball-sized bruise.”
Warfarin vs. DOACs: Different Rules
Not all blood thinners are the same. Warfarin requires regular blood tests (INR). DOACs-like rivaroxaban, apixaban, dabigatran-don’t. That changes how you prepare.Warfarin users: Check your INR within 48 hours before vaccination. If it’s above 4.0, delay the shot. Your doctor might temporarily lower your dose. A 2023 American Society of Hematology study found patients with INR >4.0 had a 37% higher chance of major bruising.
DOAC users: No INR needed. But timing matters. If you take your pill in the morning, schedule your vaccine in the afternoon. That way, drug levels are lower at the time of injection. Don’t skip your dose. Just time it right.
Some patients on DOACs are told to stop their medication before a shot. Don’t do that unless your doctor says so. Stopping even for a day increases your risk of stroke or clotting more than a bruise ever could.
What to Do After the Shot
Even with perfect technique, you might still get a small bruise. That’s normal. But if it grows, feels warm, or you can’t move your arm, call your doctor. Here’s what to expect:- Minor bruising: A dime-sized mark that fades in 3-5 days. Ice it for 15 minutes at a time if it’s sore.
- Large hematoma: A swelling bigger than a golf ball, painful, or spreading. This needs medical attention. Don’t wait.
- Extended bleeding: If blood keeps seeping after 10 minutes of pressure, apply a pressure bandage and call your clinic.
Don’t take aspirin, ibuprofen, or naproxen after the shot. These can make bleeding worse. Use acetaminophen (Tylenol) for pain if you need it.
How to Make Sure Your Provider Knows
One of the biggest problems? Providers don’t always know you’re on blood thinners. A 2023 survey found 29% of patients said their vaccinator didn’t adjust their technique-even though the patient had disclosed it.Here’s how to protect yourself:
- Bring a list of your medications. Include the name and dose.
- Wear a medical alert bracelet or wristband if you have one. Some clinics now use “Blood Thinner Alert” bands.
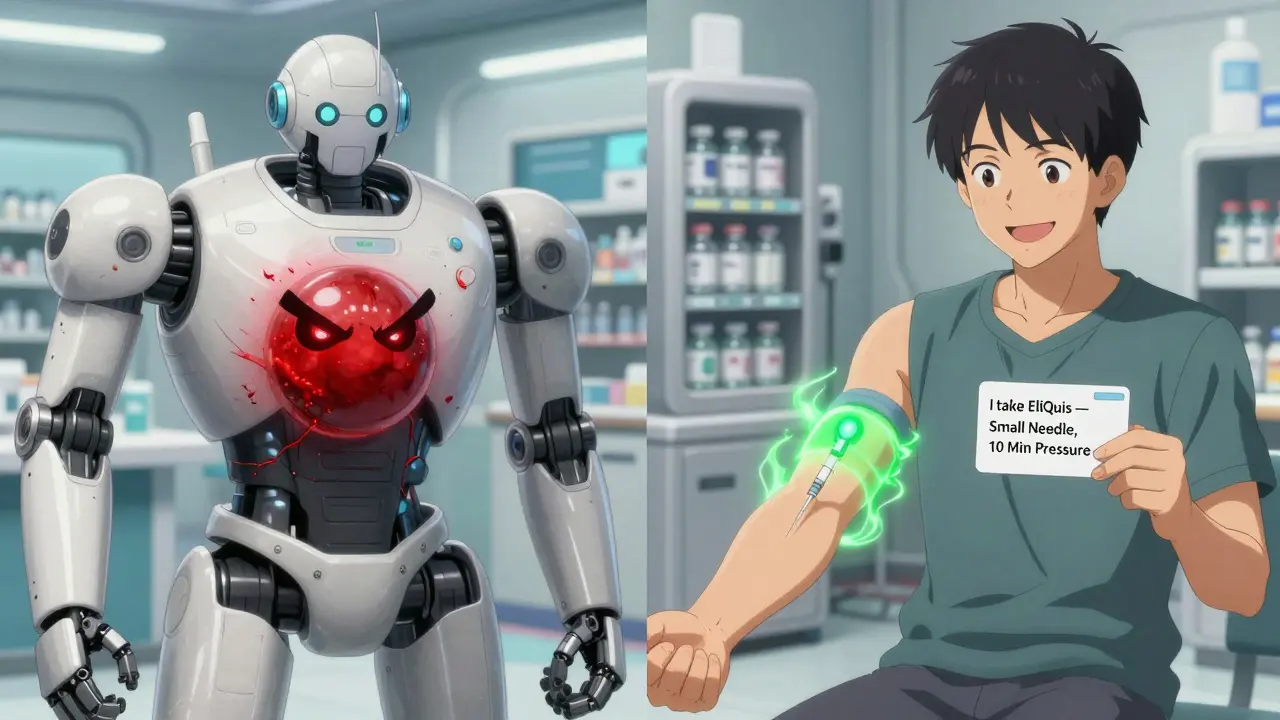
- Say it clearly: “I’m on a blood thinner. I need a small needle and 10 minutes of pressure.”
- Ask: “Do you have a 23-gauge or 25-gauge needle?” If they say no, reschedule or go to a pharmacy that specializes in immunizations.
Pharmacies like Chemist Warehouse, Priceline, or your GP’s office are often better trained than busy ERs or walk-in clinics. They vaccinate hundreds of people on anticoagulants every month.
What Happens If You Don’t Get Vaccinated?
This is the part no one talks about enough. People on blood thinners are often older and have heart disease, diabetes, or lung conditions. That makes them far more likely to get seriously ill-or die-from the flu, pneumonia, or COVID-19.According to CDC data, only 68% of adults over 65 on anticoagulants get their annual flu shot. That’s far too low. The risk of hospitalization from the flu is 5 to 10 times higher in this group than in healthy adults. And the risk of death? Even higher.
Skipping the vaccine because you’re afraid of a bruise is like avoiding a seatbelt because you’re worried about a minor scrape. The real danger is what happens if you get sick.
Real-World Success Stories
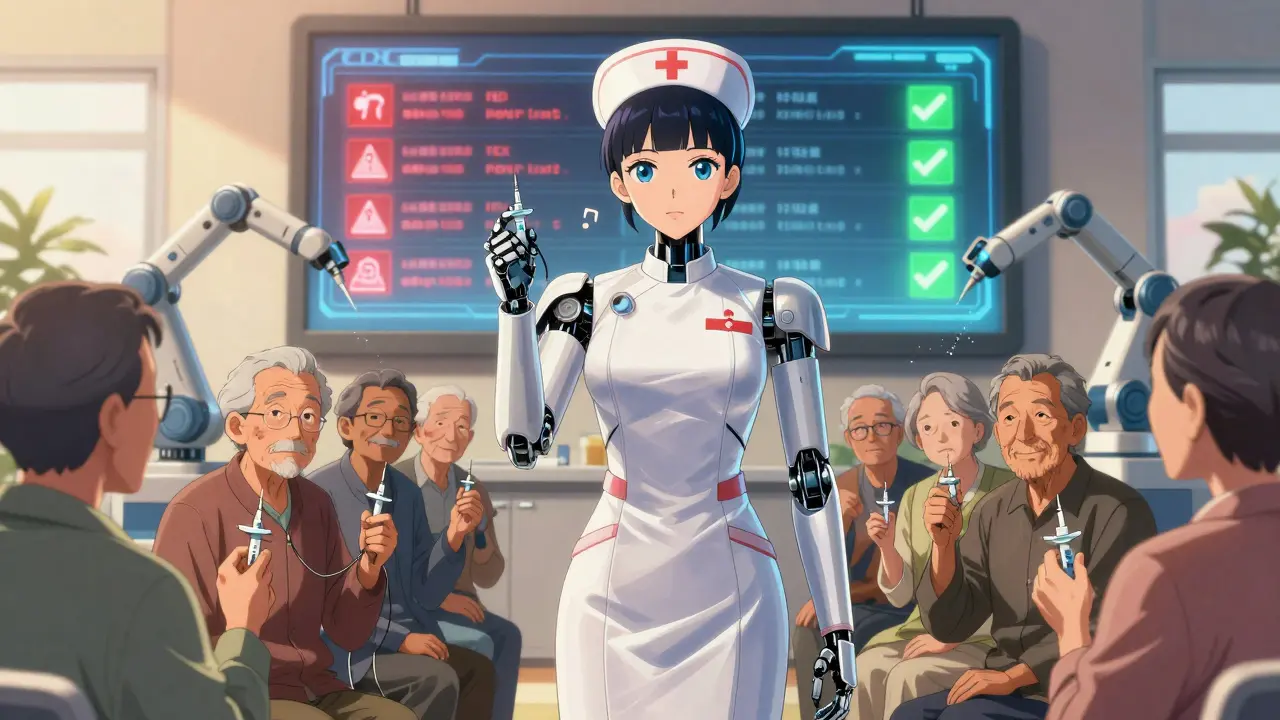
Kaiser Permanente rolled out a system-wide protocol in 2020: small needles, 10-minute pressure, staff training. Within a year, injection site complications dropped by 54%. That’s over 6,000 fewer hematomas in just one health system.At the University of Michigan’s anticoagulation clinic, they now hand out laminated cards to patients: “My name is [name]. I take [medication]. I need a 23-gauge needle and 10 minutes of pressure after my shot.” Patients show it to the nurse. Result? Nearly zero complications.
One 72-year-old woman in Sydney told her nurse: “I’ve had three big bruises from shots. I’m not doing this again.” The nurse used a 25-gauge needle, pressed for 10 minutes, and gave her a cold pack. She came back two weeks later: “Zero bruising. I’m getting my next one here.”
Bottom Line
You don’t have to choose between safety and protection. With the right needle, the right pressure, and clear communication, you can get vaccinated safely-even on blood thinners. The risk of a bad bruise is small. The risk of a bad outcome from a preventable disease? Much bigger.Don’t let fear stop you. Ask for the right technique. Insist on pressure. And get your shot.
Can I get vaccinated if I’m on warfarin?
Yes, you can. Make sure your INR is below 4.0 or within your doctor’s target range. Use a small needle (23-gauge or smaller) and apply firm pressure for at least 10 minutes after the shot. Don’t skip your warfarin dose.
Do DOACs like Eliquis or Xarelto need special handling?
No blood tests are needed. But timing matters. Take your dose after the shot if you usually take it in the morning. Use a 23-gauge needle and apply pressure for 5-10 minutes. Never stop your DOAC unless your doctor tells you to.
Should I avoid vaccines if I’ve had big bruises before?
No. Past bruising doesn’t mean you can’t get vaccinated. It means you need better technique. Ask for a smaller needle and longer pressure. Most people who switch to proper protocol have zero issues going forward.
Can I take painkillers after the shot?
Avoid ibuprofen, aspirin, or naproxen-they can increase bleeding. Use acetaminophen (Tylenol) instead if you need pain relief.
What if my doctor says I shouldn’t get the vaccine?
Ask why. Most doctors support vaccination. If they say no, ask for a referral to an anticoagulation specialist or pharmacist. The CDC, American Heart Association, and Anticoagulation Forum all say vaccines are safe and recommended for people on blood thinners.

Steven Destiny
Stop being scared of a little bruise. You’re on blood thinners because you’re at risk of a stroke-not a puffy arm. Get the shot. Use a small needle. Hold pressure. Done. Your life matters more than a purple mark.
Sophia Daniels
Oh honey. Let me paint you a picture. I had a 72-year-old aunt who refused her flu shot because she got ‘a grapefruit-sized bruise’ from a 21-gauge needle. She got the flu. Ended up in ICU for three weeks. Now? She carries a laminated card that says ‘SMALL NEEDLE. 10 MINUTES. NO RUBBING.’ And guess what? Zero bruises. Zero drama. Just peace. Stop being a victim of bad nursing. Be the person who demands better.
Pharmacies aren’t just for pills-they’re for people who refuse to be treated like cattle. Go there. Bring your meds list. Say it loud. You’re not being difficult. You’re being smart.
And if your doctor says ‘it’s fine’? Ask them if they’ve ever seen a hematoma the size of a softball. If they haven’t, they’re guessing. You’re not.
Sumler Luu
I appreciate this so much. My dad’s on Xarelto and had a bad experience last year-big bruise, couldn’t lift his coffee cup for a week. We switched to the pharmacy next to the grocery store. They used a 25-gauge, held pressure for 10 minutes, and gave him a cold pack. No issues since. It’s not rocket science. Just respect.
Brittany Fuhs
It’s alarming how many healthcare professionals still operate in the 1990s. The CDC has clear guidelines. The Anticoagulation Forum has issued position papers. And yet, nurses are still using 21-gauge needles like they’re drawing blood for a panel. This isn’t negligence-it’s systemic incompetence. Patients shouldn’t have to educate their providers. But here we are.
And while we’re at it, why isn’t there a standardized ‘Blood Thinner Vaccination Protocol’ sticker on every vaccine vial? A QR code that links to the correct technique? We have barcode scanners for everything else. Why not this?
It’s not about fear. It’s about dignity. And dignity isn’t optional.
Nikki Brown
Wow. Just… wow. Someone finally wrote this the way it needs to be said. I’ve been telling people for years: ‘Don’t skip the vaccine because you’re scared of a bruise.’ That’s like refusing to wear a seatbelt because you don’t like the feeling of the strap. You’re not protecting yourself-you’re playing Russian roulette with your heart.
And if you’re on warfarin and your INR is over 4.0? You’re not ‘being cautious.’ You’re being dangerously ignorant. Get it checked. Adjust. Don’t gamble with your life because you’re too lazy to call your doctor.
Also-NO IBUPROFEN. I’m serious. I’ve seen people take Advil after a shot and bleed out internally. Acetaminophen. Only. That’s not a suggestion. That’s a rule.
Peter sullen
Per the 2023 American Society of Hematology (ASH) Clinical Practice Guidelines, and corroborated by the Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP), intramuscular vaccination in anticoagulated patients necessitates adherence to a multimodal risk-mitigation protocol: (1) needle gauge optimization (≤23G), (2) non-aspiration technique, (3) prolonged mechanical compression (≥5–10 min), and (4) avoidance of NSAIDs post-injection. Deviation from this protocol is associated with a statistically significant increase in hematoma incidence (OR: 3.2; 95% CI: 2.1–4.8). Furthermore, DOAC timing relative to dosing window (i.e., post-dose administration) demonstrates a 41% reduction in localized bleeding events, per a prospective cohort study (n=1,204) conducted at the University of Michigan.
Therefore, clinical efficacy and patient safety are non-negotiable. Patient advocacy must be institutionalized-not anecdotal.
Fabio Raphael
I’ve been on Eliquis for 4 years. Got my last shot at a CVS last month. The pharmacist asked if I was on blood thinners, then said, ‘Oh good, we’ve got the 25s in back.’ She held pressure for 10 minutes, didn’t even ask if I wanted ice. Just did it. No fuss. I cried a little. Not because it hurt-because someone finally treated me like a person, not a risk factor.
Amy Lesleighter (Wales)
just use the small needle and press. thats it. no need to overthink. people get scared and then they dont get shots. that’s the real problem. you dont need a card or a lecture. you need a nurse who knows what to do. and if they dont? find one who does.
Rajni Jain
My mom’s from India and she was so scared of shots after one bad experience. I printed out this whole post and showed her. She took it to her doctor. They used a small needle, held pressure, and even gave her a sticker after. She said, ‘Now I feel safe.’ That’s what this is about-not just medicine. It’s about trust.
Becky Baker
Look, if you’re on blood thinners and you’re still skipping vaccines because you’re scared of a bruise, you’re letting fear win. We’re Americans. We don’t let bureaucracy or bad nurses scare us. Get the shot. Demand the right needle. Hold the pressure. And if someone gives you attitude? Walk out. There’s a Walgreens 2 miles away that does this right. We don’t settle for less here.