Melanoma Clinical Trial Eligibility Checker
Check Your Trial Eligibility
This tool estimates your potential eligibility for melanoma clinical trials based on your medical information. It's not a guarantee of eligibility - always consult with your oncologist for official screening.
When we talk about Melanoma is a dangerous form of skin cancer that originates in pigment‑producing cells called melanocytes, the first thing that comes to mind is a disease that claims thousands of lives each year worldwide. Yet, many patients never hear about the lifeline that can change that story: Clinical trial, a systematic research study that tests new medical interventions in humans under controlled conditions. Understanding why these studies matter is the first step toward better outcomes for anyone facing a melanoma diagnosis.
What Makes Clinical Trials Essential?
Every breakthrough drug, vaccine, or diagnostic tool you hear about today started as a hypothesis in a lab. Clinical trials turn those hypotheses into proven therapies. In melanoma, where survival rates have historically lagged behind other cancers, trials have been the engine that drove the rise of immunotherapy and targeted medicines.
- Evidence‑based validation: Trials generate the data regulators need to approve new treatments.
- Safety monitoring: Researchers can spot rare side‑effects before a drug reaches the general market.
- Access to cutting‑edge care: Patients enrolled in a trial often receive therapies not yet available elsewhere.
In fact, the introduction of checkpoint inhibitors in 2011 raised five‑year survival for stage III melanoma from under 30% to more than 50% - a change that would have been impossible without rigorous trial data.
Clinical Trial Phases Explained
Melanoma studies follow the same four‑phase structure used across oncology. Knowing the purpose of each phase helps patients and clinicians make informed decisions.
| Phase | Primary Goal | Typical Participant Count | Common Endpoints |
|---|---|---|---|
| Phase I | Assess safety and dosage | 20-100 | Adverse events, pharmacokinetics |
| Phase II | Evaluate efficacy and continue safety monitoring | 100-300 | Response rate, progression‑free survival |
| Phase III | Confirm benefit over standard of care | 300-3,000 | Overall survival, quality of life |
| Phase IV | Post‑approval surveillance | Thousands, real‑world populations | Long‑term safety, rare side‑effects |
Most landmark melanoma advances - such as the BRAF inhibitors vemurafenib and dabrafenib - succeeded in Phase II and Phase III trials that enrolled hundreds of patients across multiple continents.
Therapies Tested in Melanoma Trials
Three categories dominate the current trial landscape:
- Immunotherapy: Drugs that unleash the immune system, like anti‑PD‑1 antibodies (pembrolizumab, nivolumab).
- Targeted therapy: Agents that block specific mutations, chiefly BRAF and MEK inhibitors.
- Combination approaches: Pairing immunotherapy with targeted drugs, or adding radiation, to improve response rates.
Each approach has distinct biomarkers - for example, BRAF V600E mutation status - that determine eligibility. Trials that stratify patients by these markers tend to show higher success rates because the therapy is matched to the tumor’s biology.
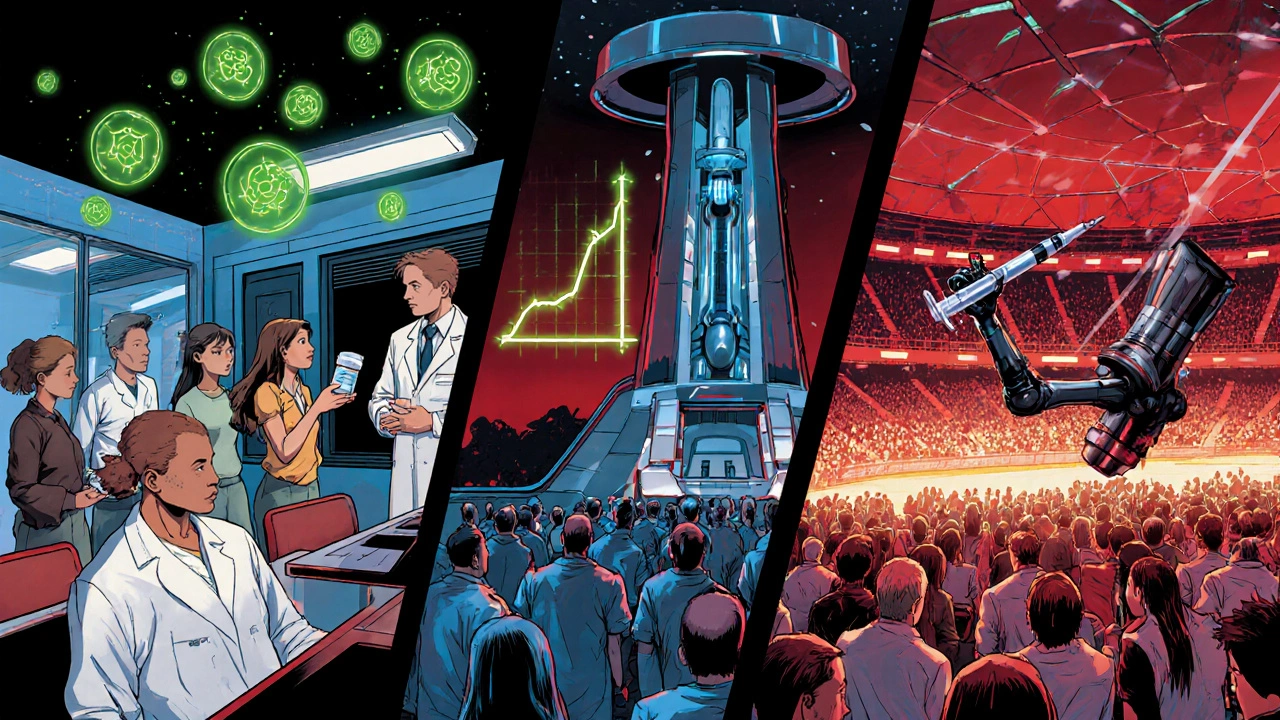
How Patients Can Get Involved
Joining a melanoma trial is simpler than many think. Here’s a quick roadmap:
- Ask your oncologist: Most dermatology‑oncology clinics have a trial navigator.
- Search registries: In Australia, the Australian New Zealand Clinical Trials Registry (ANZCTR) lists active studies; globally, ClinicalTrials.gov is the go‑to source.
- Check eligibility criteria: Age, stage, prior therapies, and genetic mutations are the most common filters.
- Consider logistics: Travel distance, trial duration, and insurance coverage can affect participation.
Patients often wonder about cost. In most high‑income countries, the trial sponsor covers the investigational drug and related medical visits, though routine care costs may still fall to the patient’s insurance.
Impact on Survival and Quality of Life
Data from recent meta‑analyses are striking. A 2023 review of 27 melanoma trials found that patients receiving checkpoint inhibitors had a 30% lower risk of death compared with standard chemotherapy. Meanwhile, BRAF‑targeted therapies reduced the median time to progression from 5 months (historical control) to 12 months in mutation‑positive cohorts.
Beyond hard endpoints, many trials now incorporate patient‑reported outcomes (PROs) to gauge quality of life. Studies that added PROs showed that patients on combination regimens reported improved fatigue scores after the first six weeks, despite higher rates of skin rash.
Challenges and Ethical Considerations
Running melanoma trials isn’t without hurdles:
- Recruitment scarcity: Advanced-stage patients may be too ill to travel to trial sites.
- Diversity gaps: Historically, trials under‑represent Indigenous Australians, African‑American, and Latin‑American populations, limiting the generalizability of results.
- Placebo ethics: In life‑threatening cancers, giving a placebo is rarely acceptable; most modern trials use an active comparator.
Regulatory bodies like the FDA and the Australian Therapeutic Goods Administration (TGA) enforce strict oversight, but researchers must also balance scientific rigor with compassionate care.
Future Directions
Next‑generation trials are reshaping how we test melanoma therapies:
- Adaptive designs: Protocols that modify dose or arm allocation based on interim results, speeding up success identification.
- Real‑world evidence (RWE): Linking electronic health records to trial data to understand effectiveness in broader populations.
- Neoadjuvant studies: Testing drugs before surgery to assess tumor shrinkage and immune activation.
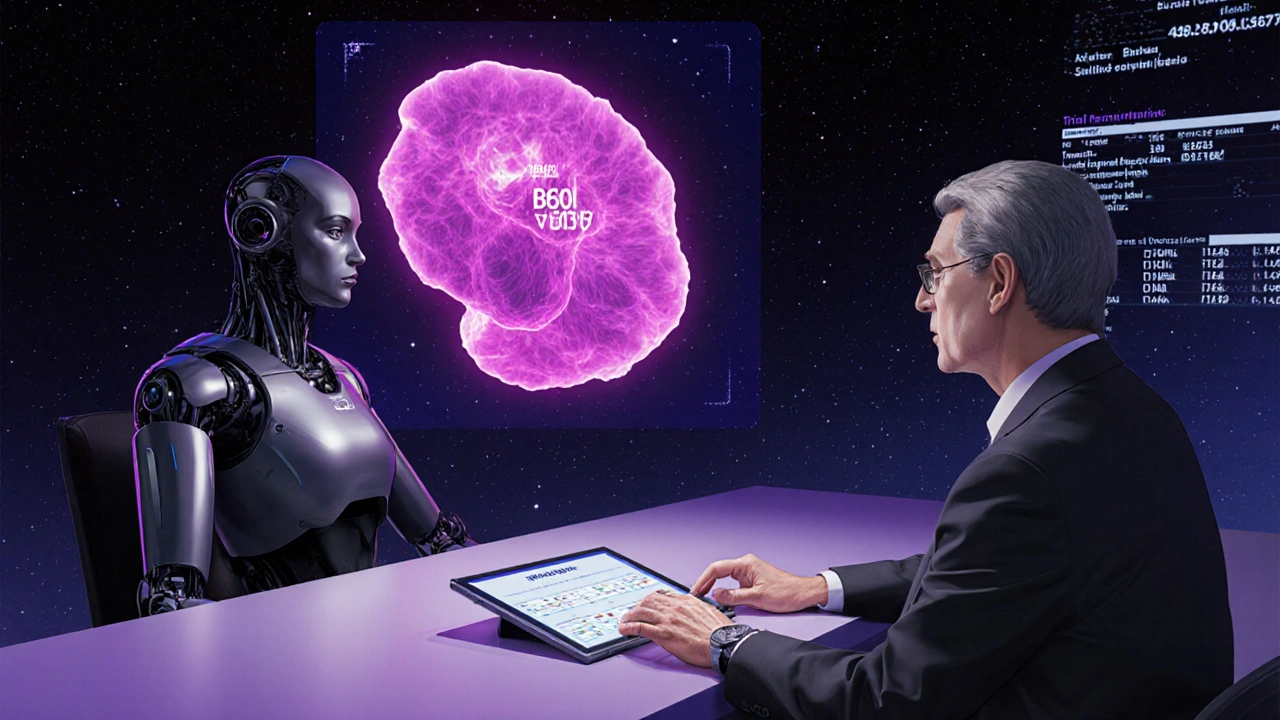
Artificial intelligence is also entering the arena, helping identify patients who are most likely to benefit from a specific trial based on genomic and imaging data. The hope is that these innovations will cut enrollment times and bring life‑saving therapies to patients faster.
Quick Takeaways
- Clinical trials provide the scientific proof that turns experimental ideas into approved melanoma treatments.
- Phase I focuses on safety, Phase II on early efficacy, Phase III on definitive benefit, and Phase IV on long‑term outcomes.
- Immunotherapy and targeted therapy dominate current melanoma research; combination trials are the new frontier.
- Patients can find trials via oncologists, ANZCTR, or ClinicalTrials.gov and should evaluate eligibility, logistics, and cost coverage.
- Recent trials have improved five‑year survival by 20‑30% and are now tracking quality‑of‑life measures alongside traditional endpoints.
Frequently Asked Questions
What is the difference between a Phase I and Phase III melanoma trial?
Phase I trials test safety and find the right dose in a small group of volunteers, while Phase III trials compare the new therapy against the current standard of care in hundreds to thousands of patients to prove real benefit.
Are clinical trial drugs free for participants?
The investigational drug and related study procedures are usually covered by the sponsor, but routine care costs such as hospital stays or standard medicines may still be billed to the patient’s insurance.
How can I find melanoma trials near me in Australia?
Start with the Australian New Zealand Clinical Trials Registry (ANZCTR) and ask your dermatologist or oncologist to check their institution’s trial listings. Many major hospitals in Perth, Sydney, and Melbourne run melanoma studies.
Do I need to have a specific genetic mutation to join a melanoma trial?
Not all trials require a mutation, but many targeted‑therapy studies look for BRAF V600E/K mutations, while some immunotherapy trials test PD‑L1 expression. The trial’s eligibility criteria will specify any required biomarkers.
What happens if I withdraw from a trial?
You can leave at any time without penalty. Your doctor will ensure you receive appropriate follow‑up care, and data already collected may still contribute to the study’s overall results.
Whether you’re a newly diagnosed patient, a caregiver, or a clinician seeking the latest evidence, recognizing the pivotal role of melanoma clinical trials is the first step toward better outcomes. By staying informed and engaging with research, you help drive the next wave of life‑saving therapies.

Alex Lineses
When we talk about melanoma research, the language of clinical trials can feel like a foreign dialect, but it's really the backbone of every new therapy.
Phase I studies are all about establishing safety and determining the optimal pharmacokinetic profile, which is why dose‑escalation cohorts are meticulously monitored.
In Phase II you start to see efficacy signals-objective response rates and progression‑free survival become the primary endpoints.
Phase III then pits the investigational agent against the current standard of care in a statistically powered, multicenter design, delivering the hazard ratios that regulators scrutinize.
Finally, Phase IV surveillance captures real‑world safety data, rounding out the evidence ecosystem that turns experimental concepts into FDA‑approved options.
kendra mukhia
Honestly, the jargon you just dropped is exactly what most patients dread-endless acronyms that mask the real human cost.
Sure, the phases sound noble, but each one also means more hospital trips, more blood draws, and more uncertainty about side‑effects.
And don’t pretend the regulatory hoops aren’t designed to protect profit motives as much as patient safety.
We need clarity, not a conference of scientists speaking in Latin.
Bethany Torkelson
Don’t sugarcoat the reality-if you stay on the sidelines while trials advance, you’re essentially betting against progress.
Grace Hada
The ethical calculus is simple: withholding access to an experimental therapy equates to an omission of beneficence.
Rohit Sridhar
I totally get how overwhelming the trial landscape can look, especially when you’re juggling appointments, insurance paperwork, and the emotional weight of a cancer diagnosis.
The first step is to lean on your care team-they’re the navigators who can match your tumor’s molecular profile with an active study.
If your melanoma harbors a BRAF V600E mutation, a targeted‑therapy trial might be the most logical avenue, whereas an immunotherapy protocol could be ideal for BRAF‑wildtype disease.
The good news is that many centers now host trial coordinators whose sole job is to demystify eligibility criteria and streamline enrollment logistics.
Geography used to be a massive barrier, but with decentralized trial models and telemedicine visits, you can often attend baseline assessments locally and still receive the investigational drug through a central pharmacy.
Financial concerns are valid, yet most sponsor contracts cover the cost of the study drug and associated monitoring visits, and you should always verify what routine care expenses remain your responsibility.
Don’t forget to ask about travel reimbursements or patient assistance programs-many pharmaceutical companies have funds earmarked for participants who need to travel long distances.
When you read a trial description, look for primary endpoints like overall survival, disease‑free survival, or patient‑reported outcome measures, because these reflect what truly matters to patients beyond just tumor shrinkage.
Adverse‑event monitoring is rigorous; you’ll have scheduled labs and imaging, but the safety team will also educate you on red‑flag symptoms that warrant immediate attention.
If you ever feel the study isn’t aligning with your goals, you have the right to withdraw without jeopardizing your standard‑of‑care treatment options.
It’s also worth noting that participation can open doors to cutting‑edge supportive care resources, such as nutrition counseling or psycho‑oncology services embedded within the trial infrastructure.
Moreover, contributing data helps the broader community-your experience may influence the next generation of combination regimens that could boost five‑year survival even further.
Remember that enrollment timelines can be fluid, with adaptive designs allowing trials to pivot based on interim efficacy signals, which sometimes accelerates approval pathways.
Stay proactive, keep a personal health journal, and maintain open communication with your oncologist to ensure you’re always on the same page about risk‑benefit considerations.
Ultimately, choosing to engage in a clinical trial is an act of hope and agency, turning uncertainty into a measurable step forward in the fight against melanoma.
Sarah Hanson
I appreciate your thorough overview; it underscores the necessity of patient‑centred communcation while also highlighting the logistical intricacies that can sometimes be overlooked.
Such clarity is invaluable for anyone navigating the complex trial ecosystem.
Nhasala Joshi
But let’s not ignore the shadowy side-big pharma’s data farms are quietly aggregating our genetic info, and the AI‑driven enrollment algorithms could be steering us toward profit‑maximizing arms instead of genuine therapeutic breakthroughs 😂🔬🚨.
Brian Van Horne
The trial ecosystem is like a finely tuned orchestra; each phase plays its part, and when the instruments sync, patients finally hear the melody of progress.
Norman Adams
Ah, yes, because nothing says 'rigorous science' like a symphony of bureaucratic paperwork and opaque eligibility charts-truly the stuff of legends.
Margaret pope
Joining a trial can be a lifeline for many patients.