Imagine this: you’ve been taking a white oval pill for your blood pressure for years. One day, your pharmacy gives you a small pink round tablet instead. No warning. No explanation. You stare at it. Is this the same medicine? Did they give you the wrong thing? You put it back in the cabinet and skip a dose. Three days later, you end up in the ER. This isn’t rare. It happens more often than you think.
Why Generic Medications Confuse People
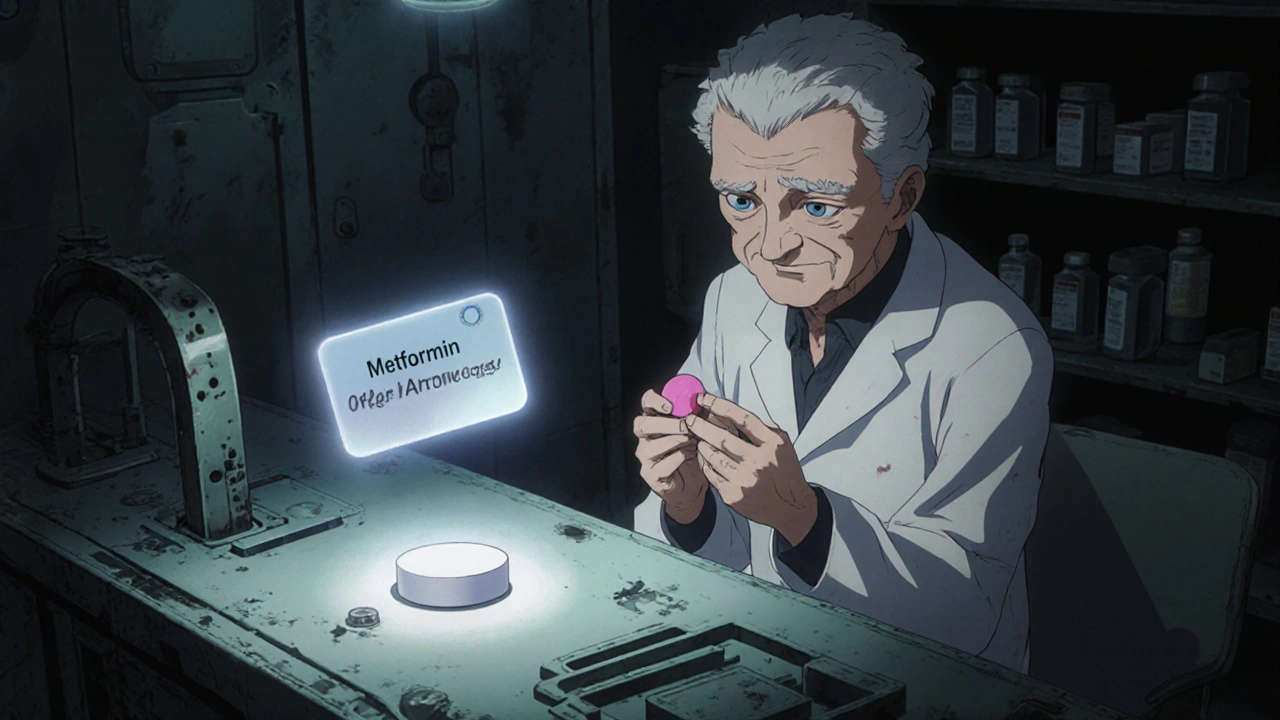
Generic drugs are chemically identical to brand-name drugs. They contain the same active ingredient, work the same way, and are held to the same safety standards. But they look different. Different color. Different shape. Different markings. And that’s where the problem starts. In the U.S., 90% of prescriptions filled are for generics. That’s because they cost less-often 80% to 85% cheaper. But for many patients, especially older adults or those with low health literacy, that difference in appearance triggers fear. A 2016 study found that 42% of patients didn’t believe generics were as effective as brand-name drugs. Even though that’s not true, the doubt sticks. Why? Because people aren’t taught how to read medication labels. They don’t know what "active ingredient" means. They don’t know that "metformin" is the same whether it’s made by Pfizer, Teva, or a little-known manufacturer. They only know what their pill looks like. When it changes, they think something’s wrong. Elderly patients managing five or six medications are especially at risk. A JAMA Internal Medicine study showed that when a generic version looked different, non-adherence jumped by 23%. That means nearly one in four patients stopped taking their medicine-not because they didn’t need it, but because they didn’t recognize it.The Real Cost of Confusion
This isn’t just about confusion. It’s about danger. Between 2015 and 2020, over 1,200 medication errors were reported because patients mixed up different generic versions of the same drug. One person took a generic blood thinner thinking it was their old pill, only to realize later it had a different dosage. Another skipped their diabetes medication because the new pill was blue instead of white. Both ended up in the hospital. Medicare data from 2022 showed that 41% of beneficiaries with multiple chronic conditions were confused by changes in their generic pills. Among those with less than a high school education, that number jumped to 63%. And here’s the kicker: 52% of older adults taking heart medications admitted to throwing away pills they didn’t recognize. They called it "pill dumping." Patients aren’t being careless. They’re being misled by a system that assumes everyone understands how generics work. But 80 million American adults have basic or below-basic health literacy. That means they struggle to read a medicine label, understand dosage instructions, or know when to call their doctor.
What Patients Need to Know
There are six key things every patient should understand about their meds-especially generics:- Name of medicine: What’s the brand name? What’s the generic name? Are they the same thing?
- What it’s for: Why are you taking this? High blood pressure? Cholesterol? Depression?
- How to take it: Once a day? With food? At bedtime?
- How to store it: Refrigerate? Keep in original bottle? Away from light?
- Side effects: What’s normal? What’s dangerous?
- When to worry: When should you call your doctor or go to the ER?
What’s Being Done to Fix This
Some solutions are already working-and they’re simple. The "Ask Me 3" program trains doctors and pharmacists to ask three questions:- What is my main problem?
- What do I need to do?
- Why is it important?

What You Can Do Right Now
You don’t need a system change to protect yourself. Here’s what you can do today:- Ask your pharmacist: "Is this the same medicine I was taking before? Why does it look different?" Don’t be shy. They’re trained to explain this.
- Keep a list: Write down the name of each medicine, why you take it, and what it looks like. Take it to every appointment.
- Use a pill organizer: If you take multiple pills, a weekly tray with labeled slots helps you spot when something’s missing or changed.
- Don’t guess: If a pill looks different and no one explained why, don’t take it. Call your doctor or pharmacy. It’s better to wait than to risk a mistake.
The Bigger Picture
This isn’t just about pills. It’s about dignity. It’s about trust. When a patient doesn’t understand their medication, they feel powerless. They start doubting their own judgment. They stop asking questions. And that’s when mistakes happen. The good news? We know how to fix this. We’ve seen it work. Clear language. Visual consistency. Pharmacist-led education. Patient-centered design. The World Health Organization says health literacy is a human right. That means no one should have to guess what their medicine is. No one should skip a dose because they don’t recognize the color. Change is coming. The FDA’s 2023 draft guidance on generic labeling is a step forward. The Biden administration’s 2023 National Action Plan sets a goal to reduce confusion-related errors by 25% by 2027. And in Europe, standardized packaging has cut errors by 27%. But real change starts with you. If you’re taking a generic, know what it is. If you’re helping someone else, ask them if they understand. And if you’re a provider-say it plainly. Don’t assume they know. Say it again. And again. Because a pill shouldn’t scare someone. It should heal them.Are generic medications as effective as brand-name drugs?
Yes. Generic medications must meet the same strict standards as brand-name drugs. They contain the same active ingredient, work the same way in the body, and are tested for safety and effectiveness by the FDA. The only differences are in color, shape, size, and inactive ingredients-none of which affect how well the medicine works.
Why do generic pills look different every time I refill my prescription?
Different manufacturers make generic drugs, and each one chooses its own color, shape, and markings. There’s no national standard for how generics must look. So if your pharmacy switches suppliers, your pill might change appearance-even though the medicine inside is exactly the same.
What should I do if my generic medication looks different?
Don’t take it until you’ve checked. Call your pharmacy and ask: "Is this the same medicine I was taking before? Why does it look different?" They can confirm it’s the correct generic and explain the change. Never assume it’s wrong-just don’t guess. Ask first.
Can I ask for the brand-name version instead of a generic?
Yes, but it may cost more. Your doctor can write "Do Not Substitute" on the prescription, which tells the pharmacy to give you the brand name. However, insurance may not cover it unless there’s a medical reason-like an allergy to an inactive ingredient in the generic. Always ask your pharmacist about costs and alternatives.
How can I avoid confusion with multiple medications?
Use a pill organizer labeled with days and times. Keep a written list of all your meds-including brand names, generic names, dosages, and what they look like. Take this list to every doctor and pharmacy visit. Apps like Medisafe can also help by letting you take a photo of each pill and storing its details.
Is it safe to stop taking a generic if I don’t recognize it?
It’s safer to stop than to take something you’re unsure about. But don’t just stop without asking. Call your pharmacy or doctor right away. They can confirm if it’s the right medication. Stopping suddenly can be dangerous for conditions like high blood pressure, diabetes, or seizures. Always get clarification before making a decision.
Leo Adi
Wow. This hit different. In India, we don’t have brand-name obsession like the US-generics are the norm, and people just learn to read the name on the strip. But I’ve seen grandmas stare at their pills like they’re alien artifacts. The color thing? Yeah, it freaks people out. No one tells them it’s the same medicine. Just… trust the system. But the system doesn’t talk back.
Melania Rubio Moreno
so like… why do they even make the pills look diffrent? like its not even a feature its a bug. i dont get it. also why is every med label written like a phd thesis??
Gaurav Sharma
The root cause is not pill aesthetics-it is systemic failure in public health education. The patient is not the problem. The infrastructure is. You cannot expect cognitive load management from individuals when the state has abdicated its duty to provide clarity. This is not negligence. It is institutional abandonment.
Shubham Semwal
bro why are people so dumb? if the name on the bottle says metformin, why do they care if it's pink instead of white? it's not like the pill is gonna turn into a frog. get a pill organizer and stop being drama queens.
Sam HardcastleJIV
One is compelled to observe that the commodification of pharmaceuticals has resulted in the depersonalization of therapeutic care. The pill, once a symbol of medical authority, has been reduced to a disposable commodity, stripped of narrative, context, and human dignity. The patient, bereft of interpretive frameworks, becomes a passive recipient of chemical randomness.
Mira Adam
It’s not about literacy-it’s about control. The system wants you confused. Confused people don’t ask questions. Confused people don’t challenge prices. Confused people take whatever’s handed to them. And that’s exactly what the pharma-industrial complex wants.
Miriam Lohrum
I think the real issue isn’t the pills changing color-it’s that we’ve stopped teaching people how to be active participants in their own care. We hand them a bottle and say ‘take this,’ but never say ‘this is why.’ We treat medicine like magic, not science. And magic is scary when you don’t understand the spell.
archana das
My aunt in Delhi used to keep her pills in a small tin with notes in Hindi-what it was for, when to take, what color it used to be. Simple. Smart. No app needed. Maybe we don’t need fancy tech-just someone to sit with them and explain. One by one.
Emma Dovener
As a pharmacist for 18 years, I can tell you: most patients don’t ask because they’re embarrassed. They think they’re stupid for not knowing. So we need to normalize the question: ‘Hey, this looks different-can you help me understand?’ That’s not ignorance. That’s wisdom.
Sue Haskett
PLEASE-every single person reading this-WRITE DOWN your meds. NAME, DOSE, WHY, WHAT IT LOOKS LIKE. Keep it in your wallet. Show it to EVERY provider. Even if they say, ‘I already know,’ show them anyway. You are your own best advocate. No one else will do it for you. Please. Please. Please.
Alex Hess
Ugh. Another ‘health literacy’ thinkpiece. Let’s be real-most people can’t even read a microwave label. This isn’t a systemic failure-it’s a biological one. Humans are bad at abstract thinking. We evolved to recognize faces, not pill imprints. Stop romanticizing ignorance. Just give people the same damn pill every time.
Jauregui Goudy
Just had a guy come in yesterday-72, on 7 meds. He showed me his pill organizer. Every slot had a sticky note with a doodle: a heart for the blood pressure pill, a sun for the vitamin D, a little lightning bolt for the diuretic. He didn’t know the names-but he knew what each one did. That’s health literacy. Not reading labels. Recognizing meaning. That’s the real win.