Some medications are like walking a tightrope. One milligram too much, and you risk serious harm. One milligram too little, and the treatment doesn’t work. These are NTI drugs - narrow therapeutic index drugs. They don’t give you room for error. Even small changes in dose or how your body absorbs them can lead to dangerous side effects or treatment failure. If you’re taking one of these, you’re not just on a medication - you’re on a high-stakes balancing act.
What Makes a Drug an NTI Drug?
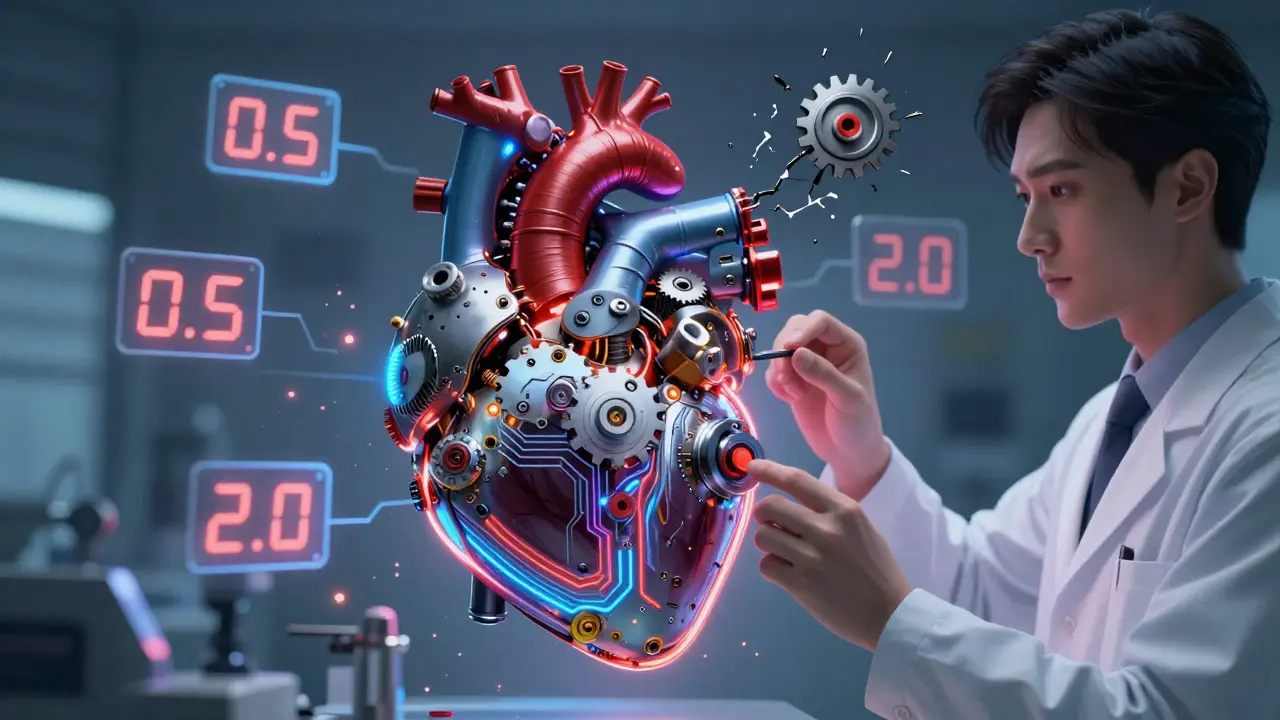
An NTI drug has a very small gap between the dose that works and the dose that harms you. The difference isn’t just small - it’s razor-thin. For example, digoxin, used for heart rhythm problems, has a therapeutic range of just 0.5 to 2.0 nanograms per milliliter in your blood. Go above 2.0, and you could get nausea, irregular heartbeat, or even cardiac arrest. Drop below 0.5, and your heart condition might flare up again. That’s less than a two-fold difference between safe and toxic levels.
The U.S. Food and Drug Administration (FDA) defines NTI drugs as those where tiny changes in blood concentration can cause serious, life-threatening problems. That’s why generic versions of these drugs aren’t treated like regular generics. For most medications, the FDA allows generic versions to differ by up to 25% in how much of the drug gets into your bloodstream. But for NTI drugs, the acceptable range is cut in half - to just 90% to 111% of the brand-name version. This tight standard exists because even a 10% difference in warfarin dose can push your INR (a measure of blood clotting) from safe to dangerous.
Common NTI Drugs You Might Be Taking
NTI drugs span multiple conditions - from heart disease to epilepsy to organ transplants. Here are the most common ones you’ll see in clinical practice:
- Warfarin - An anticoagulant used to prevent strokes and blood clots. Its target INR is 2.0-3.0. If your INR hits 4.0 or higher, your risk of major bleeding increases more than sevenfold.
- Digoxin - Used for heart failure and atrial fibrillation. The therapeutic range is 0.5-2.0 ng/mL. Toxicity can cause confusion, vomiting, and fatal arrhythmias.
- Lithium - A mood stabilizer for bipolar disorder. Safe levels are 0.6-1.2 mmol/L. Levels above 1.5 can cause tremors, confusion, kidney damage, or seizures.
- Phenytoin - An antiseizure drug. Therapeutic range: 10-20 mcg/mL. Too high? You could develop slurred speech, dizziness, or even coma. Too low? Seizures return.
- Tacrolimus - An immunosuppressant used after organ transplants. Trough levels must stay between 5-15 ng/mL. Even a 20% drop can trigger organ rejection.
- Carbamazepine - Another seizure medication. Effective range: 4-12 mcg/mL. Levels above 15 mcg/mL can cause drowsiness, double vision, or low sodium.
- Levothyroxine - Used for hypothyroidism. While TSH levels (0.5-4.5 mIU/L) are monitored, not blood levels of the drug itself, even a 12.5 mcg change can throw your thyroid balance off for weeks.
- Valproic Acid - Used for seizures and migraines. Therapeutic range: 50-100 mcg/mL. Toxicity can cause liver damage, pancreatitis, or brain swelling.
Some newer cancer drugs are also being classified as NTI. Axitinib, ponatinib, and olaparib - all targeted therapies - have very tight therapeutic windows. Their blood concentrations must be kept within narrow ranges to kill cancer cells without destroying healthy tissue.

Why Generic Substitutions Can Be Risky
Many people assume generics are interchangeable with brand-name drugs. For most medications, that’s true. For NTI drugs, it’s not always safe.
In 2023, a Reddit thread from a pharmacist described a 62-year-old woman who switched from one brand of levothyroxine to a generic. Her TSH jumped from 1.2 to 8.7 mIU/L - a massive shift. She developed fatigue, weight gain, and depression. It took three months of careful dose adjustments to get her back in range. This isn’t rare. Studies show that up to 30% of patients on levothyroxine experience noticeable changes after switching generics.
That’s why 47 U.S. states have laws restricting automatic substitution of NTI drugs. In 28 of them, a doctor must specifically write “dispense as written” or “no substitution” on the prescription. In North Carolina, the official NTI list includes digoxin, lithium, phenytoin, tacrolimus, and warfarin - and pharmacists can’t swap them without permission. Oklahoma’s 2025 list adds nortriptyline and esketamine to that group.
The European Medicines Agency takes a similar stance. Even though some newer anticoagulants like apixaban are considered safer than warfarin, the Institute for Safe Medication Practices still warns that they fall into the NTI category due to bleeding risks.
Monitoring Is Non-Negotiable
If you’re on an NTI drug, regular blood tests aren’t optional - they’re essential. Here’s what monitoring typically looks like:
- Warfarin: INR checked every 3-5 days after starting, then weekly until stable, then every 4-6 weeks.
- Lithium: Blood levels checked every 3-6 months, or sooner if symptoms change.
- Tacrolimus: Trough levels checked 3 times a week in the first month after transplant, then weekly, then monthly.
- Phenytoin: Trough levels checked at least every 2-4 weeks, especially if you’re on other medications that interact with it.
- Digoxin: Levels checked after starting, after dose changes, and if you develop nausea or dizziness.
Each test costs between $25 and $150. Medicare covers 80% for approved NTI drugs, but out-of-pocket costs still deter some patients. A 2022 study in JAMA Internal Medicine found that 32% of lithium patients miss at least one monitoring appointment per year. That’s dangerous.
Hospitals are starting to use AI tools to help. A 2022 pilot across 12 U.S. hospitals used AI to predict when a patient’s drug level was about to go out of range. It cut NTI-related adverse events by 28%. But only 45% of hospital systems have alerts built into their electronic records to flag out-of-range levels automatically.
What You Can Do to Stay Safe
If you’re on an NTI drug, here’s how to protect yourself:
- Know your drug. Ask your doctor or pharmacist: “Is this an NTI drug?” If yes, treat it like a precision tool - not a regular pill.
- Stick to one brand. If your doctor prescribes a specific brand, ask them to write “dispense as written.” Don’t switch generics unless your provider approves it.
- Never skip blood tests. Even if you feel fine, levels can drift. Missing one test could mean the difference between safety and crisis.
- Watch for interactions. Antibiotics, antifungals, even grapefruit juice can change how your body processes NTI drugs. Always tell every provider you see what you’re taking.
- Track symptoms. For lithium: tremors, confusion, frequent urination. For warfarin: unusual bruising, dark stools, headaches. Report them immediately.
There’s also promising research ahead. The NIH is funding a $15 million study using genetic testing to predict the right dose of warfarin and phenytoin for each person. Early results show a 40% faster time to reach safe levels. In the future, wearable sensors might track drug levels in real time, adjusting doses automatically.
The Bigger Picture
NTI drugs make up only about 15% of all medications that require blood monitoring - but they cause 30% of all dosing-related hospitalizations. That’s not because doctors are careless. It’s because the margin for error is so small.
The global market for NTI drugs was $48.7 billion in 2022 and is expected to hit $72.3 billion by 2028. Why? Because more targeted cancer drugs, immunosuppressants, and psychiatric medications are being developed with narrow windows. Precision medicine is here - and it demands precision dosing.
If you’re on one of these drugs, you’re part of a group that needs extra care. But with the right monitoring, communication, and awareness, you can manage it safely. Don’t assume your pharmacist can swap your medication. Don’t skip your blood tests. And don’t ignore symptoms - even if they seem minor. In the world of NTI drugs, small things matter a lot.
Gregory Parschauer
Let’s be real - this isn’t about ‘narrow therapeutic windows,’ it’s about pharmaceutical greed masked as science. The FDA lets generics slide 25% for most drugs but cuts it to 11% for NTIs? That’s not safety - that’s a cash grab. Brand-name companies lobby to keep generics out so they can keep charging $500 for a 30-day supply of levothyroxine. Meanwhile, patients are forced to pay out-of-pocket for blood tests every month like it’s some kind of wellness subscription. This system is rigged, and you’re all just parroting the pharma talking points like trained parrots.
Anny Kaettano
As someone who’s been on lithium for 12 years, I can’t stress this enough: don’t skip your labs. I missed one test because my insurance denied coverage - turned out my level was at 1.8. I was dizzy, nauseous, and nearly hospitalized. Now I keep a spreadsheet. I track my meds, my sleep, my sodium intake, even my coffee consumption. It’s not just about the drug - it’s about your whole body’s ecosystem. And yes, it’s exhausting. But it’s worth it. You’re not just taking a pill - you’re managing a delicate dance. And if you’re lucky, you’ve got a good pharmacist who actually calls you when your INR’s off.
Kimberly Mitchell
This whole post reads like a pharmaceutical white paper. Nobody cares about the 90-111% range. What matters is that your doctor is lazy, your pharmacist doesn’t know the difference between digoxin brands, and your insurance won’t cover the brand. Stop overcomplicating it. Just test your levels and don’t switch meds unless your prescriber tells you to. That’s it. The rest is noise.
Angel Molano
Stop swapping generics. Period. Your life isn’t a cost-cutting experiment.
Clay .Haeber
Oh wow. A 15% margin of error? How quaint. In my world, we call that ‘a death sentence with a pharmacy receipt.’ I mean, really - we’re letting algorithms and bureaucrats decide whether your brain stays intact? Next thing you know, they’ll be automating insulin doses with a TikTok algorithm. At least back in the day, your doctor knew your name and didn’t treat you like a data point in a Bloomberg terminal. Now we’re all just bio-robots waiting for our next blood draw like it’s a Starbucks loyalty stamp.
Avneet Singh
Interesting. But you’re ignoring the pharmacoeconomic reality. In India, even brand-name NTI drugs are often counterfeit or substandard. Monitoring is a luxury. Patients take what’s available - and survive. The Western obsession with precision is a privilege. We don’t have the luxury of 12 blood tests a year. We have one: ‘Are you still breathing?’
Adam Vella
It is worth noting that the concept of the narrow therapeutic index is not merely a pharmacological observation, but a manifestation of the epistemological limits of pharmacokinetic modeling in heterogeneous human populations. The variability in CYP450 enzyme expression, renal clearance, protein binding affinity, and gut microbiome composition renders the notion of a ‘standard dose’ a statistical abstraction - one that, when applied dogmatically, constitutes a form of biomedical authoritarianism. The patient, in this paradigm, becomes a vessel for algorithmic governance rather than a subject of clinical care.
Angel Tiestos lopez
bro. i just took my lithium and now i’m vibin’ 😌 but also kinda scared lmao
like… what if my body just… decides today’s the day it hates me?
my mom says i’m ‘too sensitive’ but what if my sensitivity is just my body screaming ‘DON’T SWITCH BRANDS’??
also why is everyone so chill about this?? i feel like i’m the only one who checks my blood levels like it’s a dating app swiping session.
also if you’re on warfarin and eat kale… you’re basically playing russian roulette with your veins. 🤯
Robin Williams
you ever think about how wild it is that we trust our lives to molecules we can’t even see?
we swallow a pill like it’s candy, then wait for a lab result to tell us if we’re alive or not.
it’s not medicine - it’s alchemy.
we’re trying to control the invisible with numbers on a screen.
and yet… we do it every day.
and somehow, people survive.
not because the system works - but because they’re stubborn.
because they show up.
because they track.
because they don’t let the bureaucracy win.
you’re not just a patient.
you’re a scientist of your own survival.
Scottie Baker
my ex switched me to generic levothyroxine ‘to save money’ - i gained 20 lbs, cried for no reason, and my hair started falling out in clumps. i had to beg my doctor to switch me back. she rolled her eyes like i was being dramatic. guess what? i’m still on the brand. and i’m not sorry. you think this is ‘healthcare’? nah. it’s a gamble. and i’m not betting my life on a $5 pill.