Medication-Food Interaction Checker
Check Your Medication's Food Requirements
Enter your medication name or select from common medications. This tool shows how food affects absorption and potential interactions based on medical research.
Select a medication to see food interaction details.
Important: This tool provides general information based on the article. Always consult your healthcare provider or pharmacist for personalized advice.
Many people pop pills without thinking about what’s on their plate. But the truth is, taking medication with food isn’t just a suggestion-it can mean the difference between feeling fine and ending up in the hospital. Whether you’re on antibiotics, blood thinners, or painkillers, what you eat-or don’t eat-when you take your medicine can change how it works in your body. And it’s not just about stomach upset. Some foods can make your drug stronger, weaker, or even dangerous.
Why Food Changes How Medicines Work
Your stomach isn’t just a place to digest burgers or salad. It’s a chemical factory that affects how drugs enter your bloodstream. When you eat, your stomach slows down. Gastric emptying, which normally takes 15 to 30 minutes on an empty stomach, can stretch to 2 to 4 hours after a meal. That extra time lets certain drugs dissolve better and get absorbed in the small intestine, where most of them are absorbed anyway. But it’s not just timing. Food changes the chemistry around your drug. Fats can help certain medications dissolve, while calcium, iron, or fiber can bind to them and stop them from being absorbed. Grapefruit juice? It shuts down an enzyme in your gut called CYP3A4, which normally breaks down drugs like statins and blood pressure meds. Without that enzyme doing its job, too much drug floods your system. Studies show that when people take medications with food when they’re supposed to, side effects drop by up to 60%. For example, non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen cause stomach ulcers in 38% of people who take them on an empty stomach. That number drops to 12% when taken with food. That’s not a small difference-it’s life-changing for someone with arthritis or chronic pain.Medications That Need Food to Work Right
Not all meds are the same. Some need food to be absorbed properly. Others need to be kept away from it. Here’s what you need to know:- Antifungals like griseofulvin: Absorption jumps 15-30% when taken with a high-fat meal. Without it, the drug just passes through you.
- NSAIDs (ibuprofen, naproxen): Food reduces stomach irritation and lowers the risk of bleeding. The Arthritis Foundation says microscopic stomach damage happens in 25% of people within 24 hours if taken empty.
- Statins like simvastatin: Taken with food? Fine. Taken with grapefruit juice? Big problem. Grapefruit can make blood levels spike 9 to 15 times higher, raising the risk of muscle damage.
- Antipsychotics like clozapine: High-fat meals can boost blood levels by 40-60%, making you dangerously sleepy or dizzy.
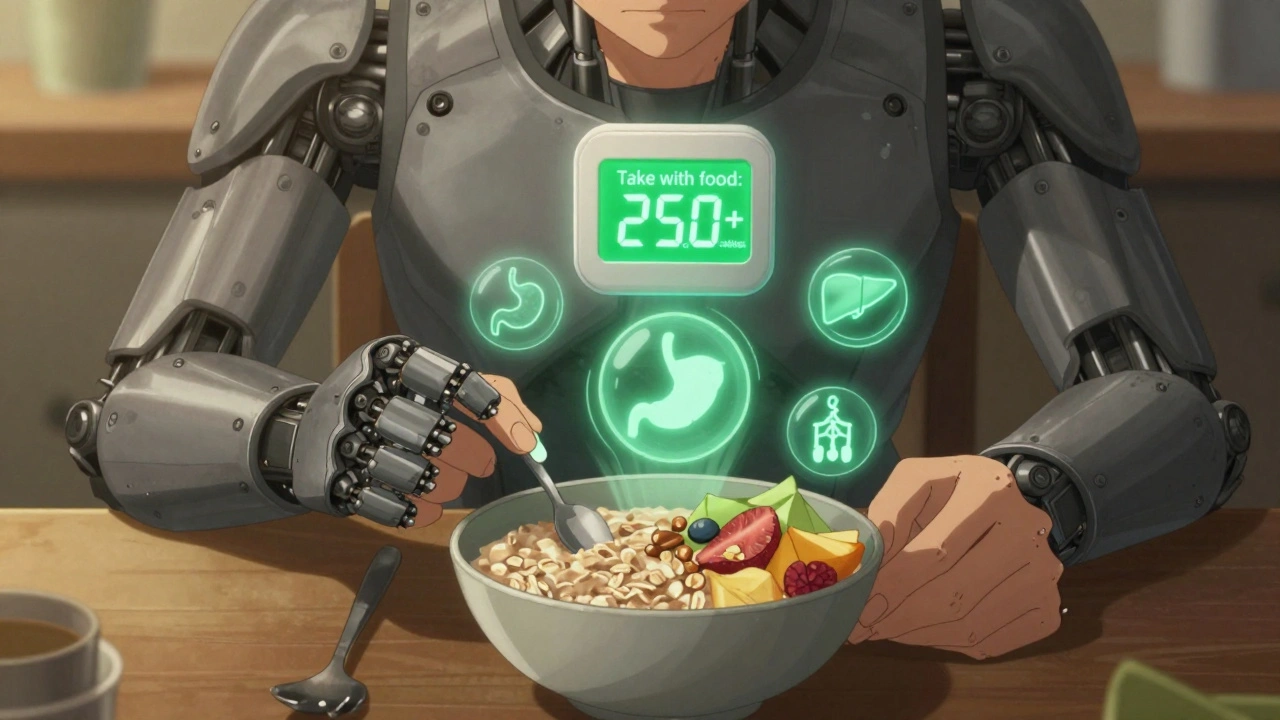
- Metformin (for diabetes): A Drugs.com analysis of 15,000 reviews found 63% of users had severe nausea or diarrhea when taken without food. With food? That drops to 18%.
These aren’t edge cases. They’re common prescriptions. If you’re on any of these, food timing isn’t optional-it’s part of the treatment.
Medications That Must Be Taken on an Empty Stomach
Some drugs work best when your stomach is empty. Food gets in the way.- Levothyroxine (for hypothyroidism): Calcium, iron, soy, or even coffee can block absorption. Studies show taking it with breakfast can cut effectiveness by 30-55%. That means your thyroid levels stay low, and you keep feeling tired, cold, or gaining weight-even if you’re taking the right dose.
- Tetracycline antibiotics: Dairy, antacids, or calcium supplements bind to this drug and reduce absorption by up to 50%. You might think you’re getting treated for an infection, but the drug isn’t even reaching your bloodstream.
- Fluoroquinolones like ciprofloxacin: Calcium in milk, yogurt, or fortified orange juice cuts absorption by half. Take it two hours before or after dairy.
- Proton pump inhibitors like omeprazole: These need stomach acid to activate. Eating right before blocks that. They should be taken 30 minutes before your first meal.
People often don’t realize this. A Mayo Clinic study found that 57% of patients taking levothyroxine admitted to swallowing it with their morning coffee and toast. That’s not harmless-it’s medically significant. Many ended up needing higher doses just to reach normal thyroid levels.
The Grapefruit Trap
Grapefruit juice is a sneaky culprit. It’s not just about one glass. The enzyme it blocks-CYP3A4-stays shut down for 24 to 72 hours. So even if you drink grapefruit juice at breakfast and take your pill at night, you’re still at risk. Drugs affected include:- Cyclosporine (used after organ transplants)
- Some blood pressure meds (like felodipine)
- Cholesterol drugs (simvastatin, atorvastatin)
- Anti-anxiety meds (like buspirone)
One study showed cyclosporine levels jumped 300-500% after grapefruit juice. That’s not a side effect-it’s a toxic overdose waiting to happen. And it’s not just grapefruit. Pomelo, Seville oranges, and some tangelos do the same thing.
Here’s the kicker: you don’t have to drink a whole glass. One small glass-about 200ml-is enough to cause problems. And if you’re on multiple meds? The risk stacks up.

What About Vitamins and Supplements?
You might think supplements are harmless. They’re not.- Calcium and iron supplements: These bind to antibiotics like tetracycline and fluoroquinolones. Take them at least 2 hours apart.
- Vitamin K: Found in spinach, kale, broccoli. It directly opposes warfarin (Coumadin). If you eat a big salad one day and no greens the next, your blood clotting levels swing wildly. A New England Journal of Medicine study found 20-30% of warfarin patients had dangerous INR fluctuations because of inconsistent vegetable intake.
- CBD oil: New research from UCLA shows high-fat meals can boost CBD absorption by 4 to 5 times. That’s fine if you’re using it for pain-but dangerous if you’re also on blood thinners or seizure meds.
Many people don’t realize their daily multivitamin or fish oil pill is interfering with their prescription. Always check with your pharmacist before adding anything new.
What Does “With Food” Actually Mean?
It’s not just “eat something.” The FDA defines “take with food” as at least 250-500 calories. That’s not a cracker. That’s a sandwich, a bowl of oatmeal with nuts, or yogurt with fruit. And “on an empty stomach”? That means 1 hour before or 2 hours after eating. No coffee, no toast, no candy. Even a sip of milk can ruin absorption for some drugs.People often think, “I had a bite of toast-should be fine.” But with levothyroxine or tetracycline, even a small amount of calcium can block the drug. That’s why timing matters more than you think.
Why So Many People Get It Wrong
You’d think doctors and pharmacists would explain this clearly. But they don’t always. A Mayo Clinic study found that 68% of patients over 65 had no idea about food-drug interactions for their medications. Only 22% got clear instructions during their prescription counseling. That’s not a patient problem-it’s a system problem. Add to that: polypharmacy. The average Medicare beneficiary takes 4-5 medications. Some need food. Some need no food. Some need to wait two hours. It’s a scheduling nightmare. One study found 34% of older adults struggle with conflicting food timing rules. And younger people? Even worse. Only 28% of patients aged 18-34 talk to their pharmacist about food interactions. They assume it’s not important-or they forget.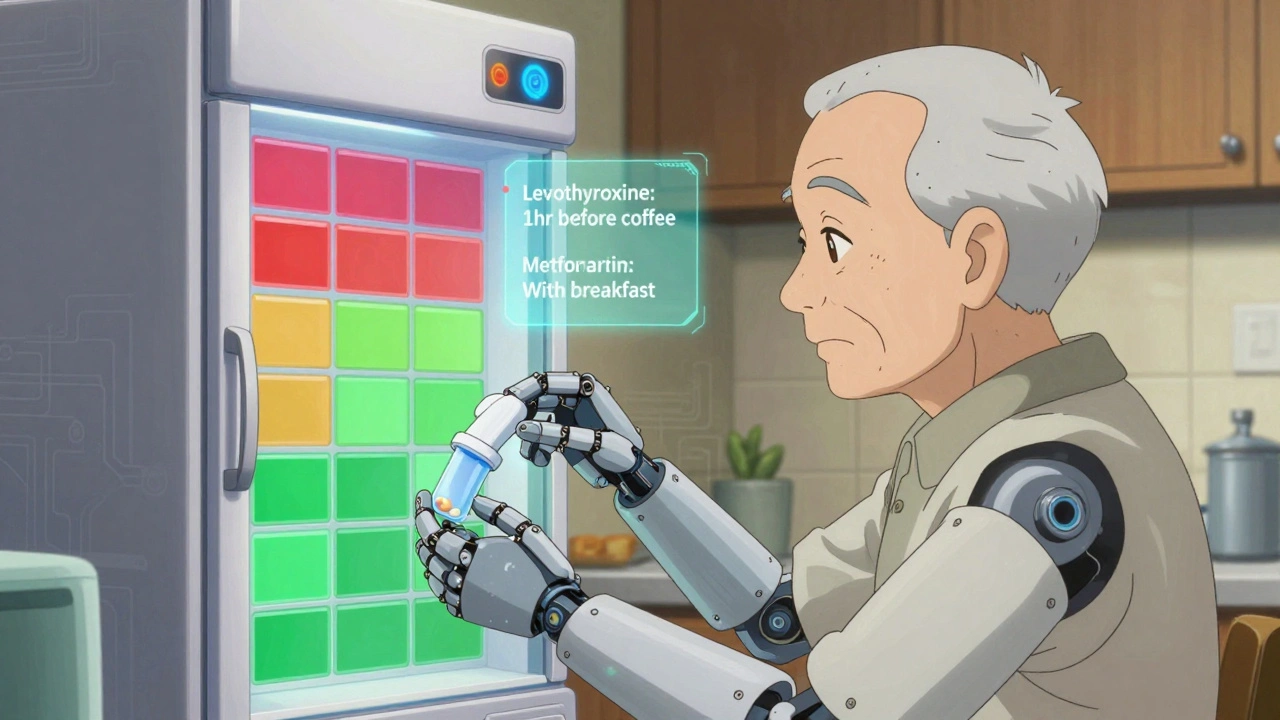
How to Get It Right
You don’t need to memorize a 50-page guide. Here’s what actually works:- Ask your pharmacist every time you get a new prescription. Say: “Should I take this with food, or on an empty stomach? What foods or drinks should I avoid?”
- Use a medication app. Apps like Medisafe send reminders not just for when to take your pill-but whether to take it before or after eating. Clinical trials show they reduce errors by 37%.
- Keep a food-drug log. Write down what you ate and when you took your meds. After a week, you’ll spot patterns. Did you feel sick after taking metformin with coffee? Did your blood pressure spike after grapefruit? Track it.
- Use color-coded charts. Many hospitals now use red (must take on empty stomach), green (take with food), and yellow (flexible) labels. You can make your own. Stick it on your fridge.
- Don’t assume. Just because one statin is safe with grapefruit doesn’t mean the next one is. Pravastatin? Fine. Simvastatin? Dangerous. Names matter.
It’s not about being perfect. It’s about being consistent. One slip-up won’t kill you-but repeated mistakes can.
The Future: Smart Pills and Personalized Advice
The field is changing fast. In March 2024, the FDA approved the first “smart pill”-Abilify MyCite-that tracks when you take your medicine and whether you ate around the same time. Early data shows a 32% drop in food-related side effects. Companies like Nutrino and Vitagene now offer DNA-based reports that tell you how your body processes drugs with certain foods-for $149 to $299. The NIH is spending $15.7 million to study how your gut bacteria affect drug absorption. By 2028, experts predict 75% of medication regimens will include personalized food timing based on genetics. Right now, it’s just 18%. But here’s the catch: as processed foods get more complex-with hidden calcium, sugar, and additives-predicting interactions gets harder. Without better education, the number of adverse events could rise by 15-20% in the next decade.Bottom Line
Taking medication with food isn’t a detail. It’s a core part of your treatment. A missed meal, a glass of juice, or a calcium supplement can turn a safe drug into a risky one-or make it useless. You don’t need to be a scientist to get it right. You just need to ask. Check the label. Talk to your pharmacist. Track your habits. And don’t assume “it’s probably fine.”The data is clear: when you match your meds with the right food-or avoid it-you reduce side effects, improve effectiveness, and avoid hospital visits. That’s not just smart. It’s essential.
Taya Rtichsheva
so i just took my ibuprofen with a single cheerio and now my stomach is doing the macarena
thanks for the warning i guess
Christian Landry
holy crap i had no idea grapefruit juice could wreck your meds for DAYS 😳
just realized i’ve been drinking it with my statin for 3 years… time to switch to orange juice… or water… or maybe just quit juice entirely 🥲
Kathy Haverly
this is why people die. doctors don’t care. pharmacists are overworked. you’re left to google your own death. and now you’re supposed to keep a food log too? great. another chore for the already exhausted. this isn’t healthcare. it’s a full-time job.
Chris Marel
i’ve been taking metformin with my rice and dal for years and never had nausea. maybe it’s the type of food? or just luck? i’ve heard stories from friends in the US who swear by taking it on empty, but here it’s just… part of the meal. wonder if culture plays a role in how drugs behave?
Evelyn Pastrana
my grandma takes 7 meds and still makes her own color-coded fridge chart. she’s 82. i’m 28 and can’t remember if i brushed my teeth. we need more of her. less of me. 🙏
Nikhil Pattni
actually the science here is oversimplified. CYP3A4 inhibition isn't just about grapefruit-it's about furanocoumarins, and the concentration varies wildly by cultivar, season, and processing. also, levothyroxine absorption is affected by gastric pH, not just calcium-so timing matters, but so does stomach acid production, which declines with age. also, your gut microbiome metabolizes drugs differently based on fiber intake, probiotics, and even stress levels. i’ve read 47 papers on this. most people don’t even know what a CYP enzyme is. and yes, apps help, but only if you actually use them. also, did you know that soy protein can interfere with levothyroxine more than dairy? nobody talks about that. and what about the 2023 meta-analysis on polypharmacy and circadian rhythms? no? well now you do. #pharmacogenomics
Elliot Barrett
this post is just a long ad for pharmacy apps. who has time for this? just take the pill. if you feel weird, stop. it’s not that hard.
Sabrina Thurn
as a clinical pharmacist, i see this daily. the real tragedy isn’t the lack of knowledge-it’s the lack of system support. patients aren’t lazy; they’re overwhelmed. we need standardized, visual, multilingual counseling tools built into EHRs-not just a 30-second verbal warning during a 10-minute visit. also, the smart pill data is promising, but cost and privacy are massive barriers. we’re not ready for personalized food-timing regimens yet. but we can start by training pharmacy techs to ask: 'what did you eat before you took this?' instead of just handing out the script.