Drug Tolerance: What It Is, Why It Happens, and How to Handle It
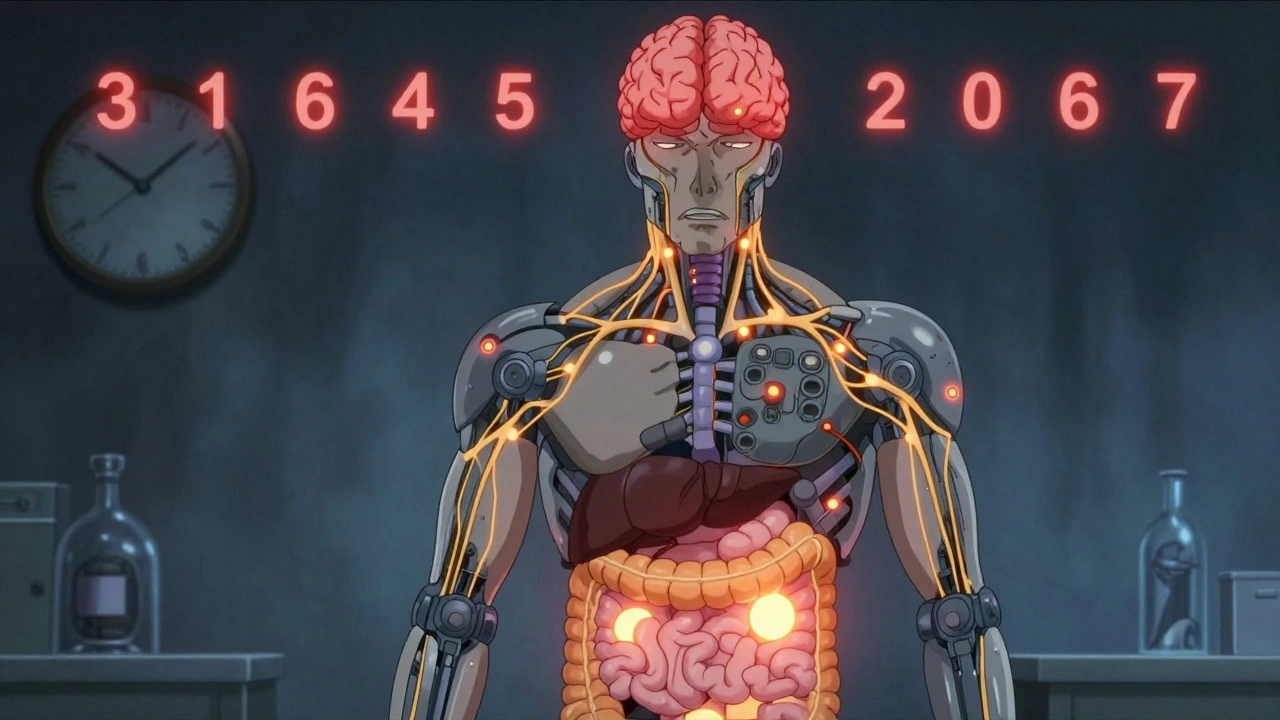
When you take a medication regularly, your body can start to adapt—this is called drug tolerance, a reduced response to a medication after repeated use, requiring higher doses to achieve the same effect. Also known as medication tolerance, it’s not the same as addiction, but it can lead to dangerous choices if not understood. You might notice it with painkillers, sleep aids, or even antidepressants. The drug still works, but not like it used to. That’s not a flaw in the medicine—it’s your body learning to cope.
Some drugs are more likely to cause tolerance than others. Opioids like oxycodone, benzodiazepines like diazepam, and stimulants like modafinil are common culprits. Even common OTC sleep aids can trigger it if used nightly for weeks. Tolerance development, the gradual decrease in drug effectiveness due to physiological adaptation happens because your cells adjust receptor sensitivity, change how they process the drug, or speed up its breakdown. It’s automatic, silent, and often unnoticed until you’re taking more than you should.
What makes it tricky is that tolerance doesn’t always mean you need more. Sometimes, stopping suddenly causes withdrawal symptoms, physical or mental reactions that occur when a drug is reduced or stopped after prolonged use—sweating, anxiety, insomnia, or even seizures. That’s why doctors don’t just crank up the dose. They look at alternatives, timing, or non-drug options. For example, if you’ve built up tolerance to a sleep med, adding good sleep hygiene might bring back the effect without increasing pills.
And here’s the thing: tolerance doesn’t mean you’re weak or doing something wrong. It’s biology. People on long-term pain meds, antianxiety drugs, or even ADHD stimulants can develop it—even when taking them exactly as prescribed. The real risk isn’t tolerance itself. It’s what people do next: doubling the dose, mixing with alcohol, or skipping doctor visits. That’s where things go off track.
Some drugs, like antibiotics, can develop resistance instead—where the bug adapts, not your body. But with most prescription and OTC meds, it’s your system changing. That’s why checking in with your pharmacist matters. They see patterns. They know which meds are most likely to cause tolerance, and they can spot when someone’s creeping up on unsafe doses.
In the posts below, you’ll find real-world examples of how tolerance shows up—with pioglitazone, esketamine, modafinil, and even sleep aids. You’ll see how people manage it, when to ask for help, and what alternatives actually work. No fluff. No theory. Just what happens when your body stops responding the way it used to—and what to do about it.
Why Some Medication Side Effects Fade Over Time: The Science of Tolerance
Learn why some medication side effects fade over time while others don't. Discover how metabolic and cellular changes cause tolerance-and what you can do about persistent effects.