Medication Tolerance: What It Is, Why It Happens, and What to Do
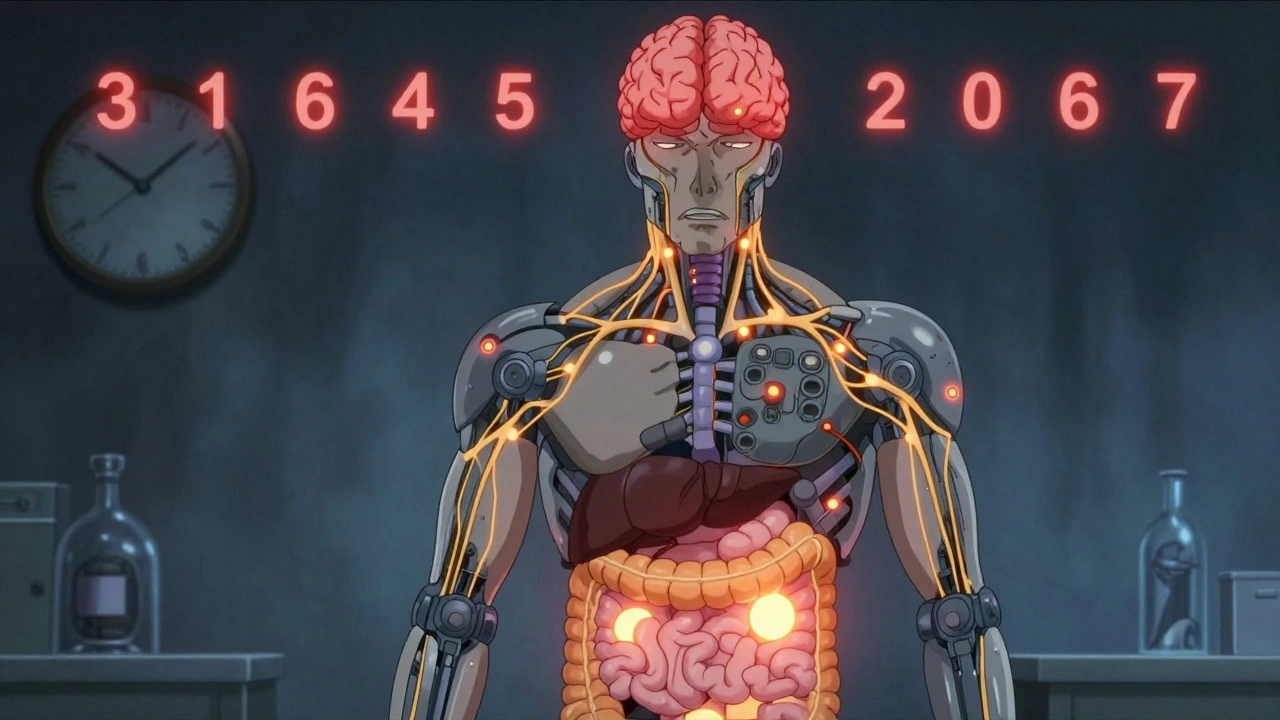
When your body gets used to a medicine and it stops working like it used to, that’s medication tolerance, a physiological adaptation where the body responds less to a drug after repeated use. Also known as drug tolerance, it’s not about addiction—it’s about biology. You might need higher doses to feel the same effect, or the drug might just stop working altogether. This happens with painkillers, antidepressants, blood pressure meds, and even sleep aids. It’s common. It’s predictable. And if you don’t know how to handle it, it can be dangerous.
Medication tolerance isn’t the same as dependence or addiction, but the two can overlap. For example, someone taking opioids for chronic pain may develop tolerance—needing more to control discomfort—while also becoming physically dependent, meaning they get withdrawal symptoms if they stop. Withdrawal symptoms, the physical and mental reactions that occur when a drug is reduced or stopped after prolonged use can include anxiety, nausea, sweating, or even seizures, depending on the drug. That’s why you never just quit cold turkey. Tolerance also affects medication effectiveness, how well a drug works at its prescribed dose to treat a condition. If your blood pressure med no longer keeps your numbers in range, or your antidepressant doesn’t lift your mood like it used to, tolerance could be the hidden cause.
Some drugs build tolerance faster than others. Benzodiazepines, stimulants, and opioids are big ones. But even common meds like proton pump inhibitors for heartburn or antihistamines for allergies can lose their punch over time. The body adapts by changing receptor sensitivity, speeding up metabolism, or reducing drug absorption. It’s not your fault. It’s not weakness. It’s science. And the good news? There are smart ways to deal with it. Doctors can adjust dosing, switch medications, or use drug holidays—short breaks under supervision—to reset your system. Sometimes, non-drug approaches like physical therapy, sleep hygiene, or stress management can help reduce reliance altogether.
What you’ll find below are real, practical posts about how tolerance shows up in everyday meds—from pioglitazone and esketamine to sleep aids and blood pressure drugs. You’ll see how sodium intake affects your prescriptions, why generic substitutions matter when tolerance kicks in, and how to spot when a drug is losing its edge before it’s too late. No fluff. No jargon. Just what you need to know to stay safe and in control.
Why Some Medication Side Effects Fade Over Time: The Science of Tolerance
Learn why some medication side effects fade over time while others don't. Discover how metabolic and cellular changes cause tolerance-and what you can do about persistent effects.