Pharmacodynamic Tolerance: What It Is and How It Affects Your Medications
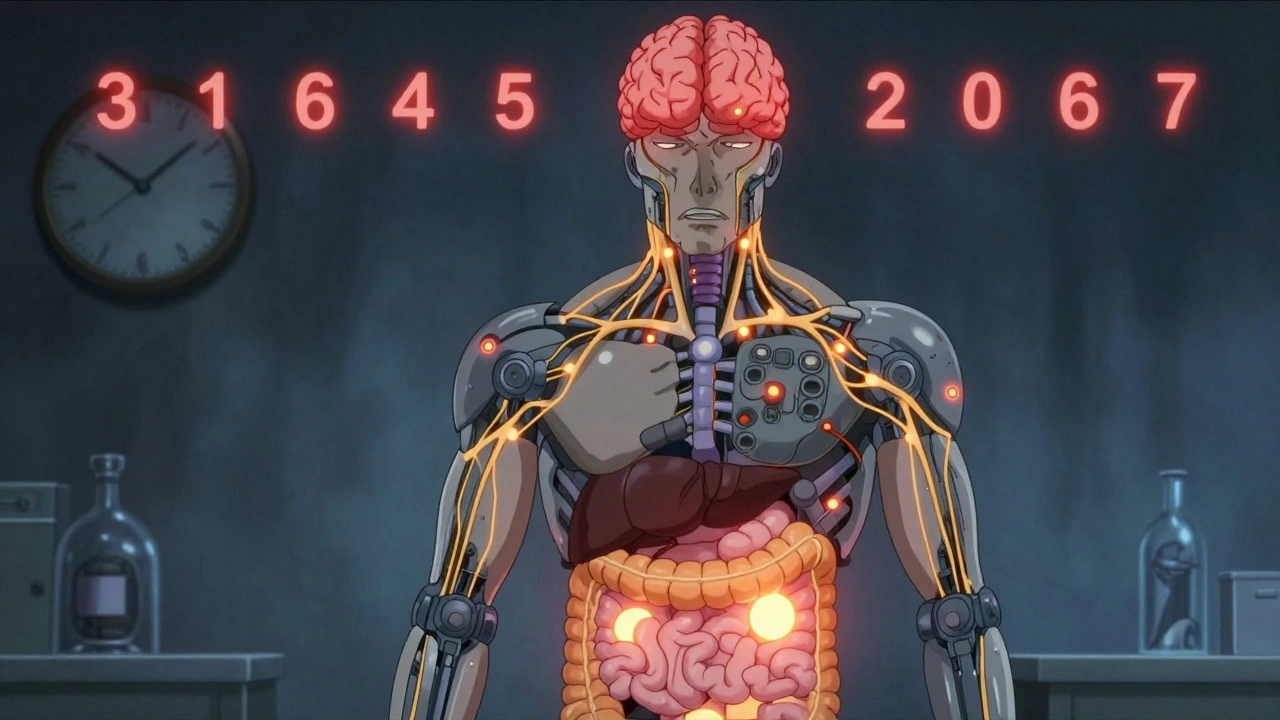
When a drug stops working like it used to, it’s not always because your body is broken—it might be pharmacodynamic tolerance, a process where your body’s response to a drug weakens over time, even at the same dose. This isn’t addiction. It’s biology. Your cells adjust. Receptors downregulate. Signaling pathways get tired. The result? You need more to feel the same effect—or you feel nothing at all.
This happens with many common drugs. opioids, used for pain, often trigger pharmacodynamic tolerance quickly. So do benzodiazepines, like Xanax or Valium, used for anxiety and sleep. Even antidepressants, including SSRIs, can lose effectiveness over months. It’s not that the drug is broken. Your body changed. And that change is measurable, predictable, and often unavoidable.
Pharmacodynamic tolerance is different from pharmacokinetic tolerance—where your body just breaks down the drug faster. Here, the problem is at the target site: your neurons, your receptors, your cellular switches. That’s why switching brands or dosing schedules doesn’t always help. The issue isn’t the pill. It’s how your cells respond to it.
Some people notice this with pain meds. Others with sleep aids. Some with anxiety drugs. And it’s not just about feeling less relief—it’s about safety. When tolerance builds, people often increase doses without knowing the risks. That’s how overdoses happen. That’s why understanding this process matters more than ever.
Below, you’ll find real-world examples of how pharmacodynamic tolerance shows up in daily medication use—from diabetes drugs that lose punch to sleep aids that stop working after a few weeks. You’ll see what doctors and pharmacists watch for, what patients miss, and how to spot the signs before things get dangerous. No fluff. Just what you need to know to stay in control of your meds.
Why Some Medication Side Effects Fade Over Time: The Science of Tolerance
Learn why some medication side effects fade over time while others don't. Discover how metabolic and cellular changes cause tolerance-and what you can do about persistent effects.