For millions of people taking statins to lower cholesterol and prevent heart attacks, muscle pain isn’t just an inconvenience-it’s a dealbreaker. About 1 in 4 patients stop their statin because of muscle aches, weakness, or cramps. And for years, many doctors have looked to one simple fix: vitamin D. The idea was appealing: if low vitamin D causes muscle problems, then fixing it might let people stay on life-saving statins. But does it actually work? The answer isn’t what you might expect.
The Promise of Vitamin D for Statin Users
Around 2009, a small study caught attention. Researchers found that 92% of patients who couldn’t tolerate statins due to muscle pain saw their symptoms vanish after taking vitamin D supplements. That number was too good to ignore. Suddenly, doctors started checking vitamin D levels in patients who complained about statin side effects. If levels were low-below 20 ng/mL-they’d prescribe supplements and try the statin again. Many patients reported feeling better. Some even got back on statins after failing multiple times before. The logic made sense. Vitamin D helps muscles function properly. Low levels are linked to weakness and pain, even without statins. Statins themselves can interfere with muscle metabolism. So, if both factors are at play, fixing vitamin D might remove one trigger. Studies from 2017 showed that patients with vitamin D levels ≤20 ng/mL had a 90% success rate in restarting statins after supplementation. Those with higher levels? Only 33% could tolerate them. That gap was hard to ignore.What the Big Study Found
But science doesn’t rely on small studies or anecdotal wins. In 2022, the JAMA Cardiology team released the first large, randomized, placebo-controlled trial-exactly the kind of study that settles debates. They followed over 2,000 people starting statins. Half got 2,000 IU of vitamin D daily. The other half got a dummy pill. After a year, there was no difference. Both groups had the same rate of muscle pain: 31%. Both groups stopped their statins at the same rate: 13%. No benefit. No protection. No improvement in tolerance. This wasn’t a fluke. The study was well-designed, funded by the NIH, and followed strict protocols. It didn’t just measure symptoms-it tracked actual drug discontinuation. And it found nothing. That’s the kind of result that changes practice.Why the Confusion? Observational vs. Real Evidence
So why did earlier studies say vitamin D helped? Because they were looking at the wrong thing. Most of the positive reports were observational. That means researchers looked at patients who already took vitamin D and noticed they seemed to tolerate statins better. But that doesn’t prove cause and effect. Think of it this way: people who take vitamin D supplements are often more health-conscious. They might exercise more, eat better, or see their doctor regularly. Maybe they’re less likely to ignore mild muscle pain and more likely to get tested. Maybe their pain improved because they rested more, not because of the vitamin D. These hidden factors-called confounders-can make a weak link look strong. The 2022 trial removed those biases. Everyone was randomly assigned. No one knew if they were getting the real supplement or a placebo. That’s the gold standard. And it showed: vitamin D didn’t make a difference.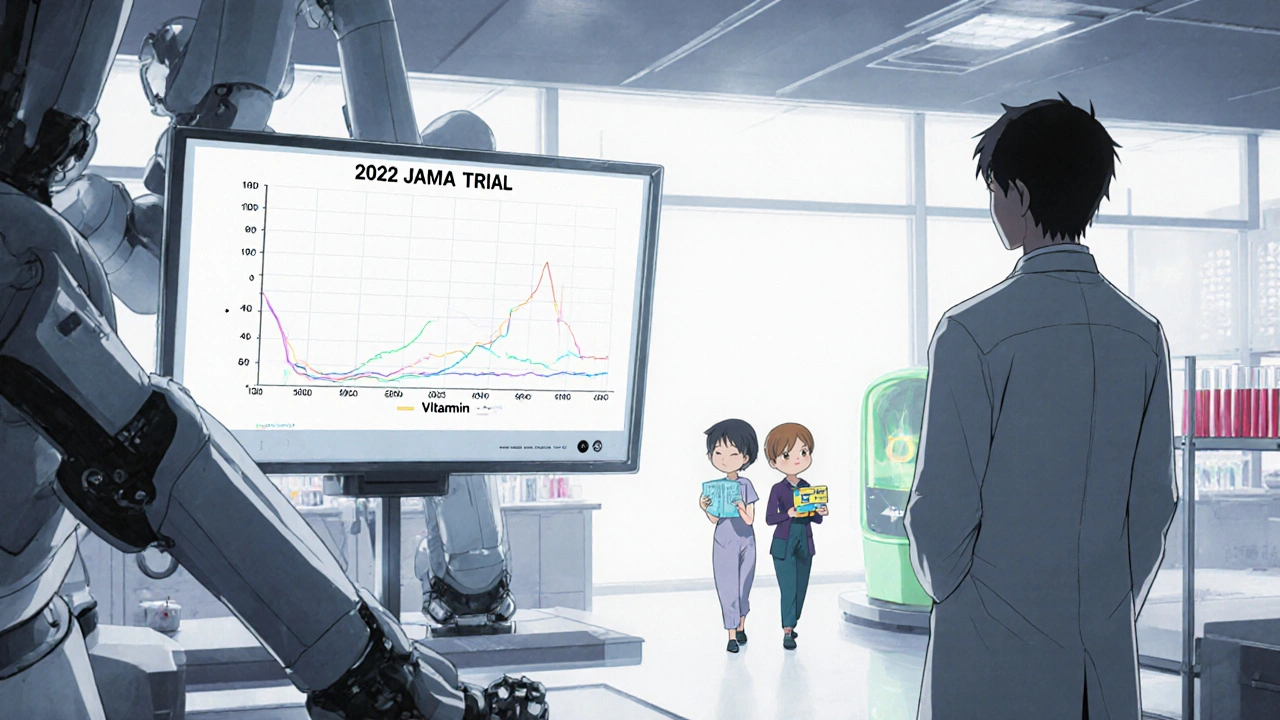
What About Statin Types and Vitamin D Levels?
Some studies suggest certain statins interact differently with vitamin D. One 2019 study found that people taking atorvastatin had higher average vitamin D levels than those on other statins. Another suggested that after correcting low vitamin D, pravastatin and rosuvastatin were better tolerated than others. But these are just patterns-no proven mechanism. It’s possible that vitamin D affects how the liver processes certain statins, especially those broken down by CYP enzymes. But even if that’s true, the 2022 trial suggests that even if there’s a biological interaction, it doesn’t translate into fewer symptoms or better adherence in real life.Should You Still Check Your Vitamin D?
Here’s the practical takeaway: vitamin D supplementation doesn’t reliably improve statin tolerance. If you’re on a statin and have muscle pain, don’t assume low vitamin D is the culprit. But that doesn’t mean you should ignore your vitamin D levels entirely. Vitamin D is still important for bone health, immune function, and overall muscle strength. If your levels are low-especially below 20 ng/mL-you should correct it. Not because it will help you take statins, but because your body needs it. Many people are deficient, especially in places like Melbourne where winter sunlight is limited. If you’ve had trouble with statins before, talk to your doctor about alternatives. Maybe a lower dose. Maybe a different statin. Maybe non-statin options like ezetimibe or PCSK9 inhibitors. Don’t skip your statin just because you’re not feeling great-work with your doctor to find a solution that actually works.
What This Means for Your Heart
Statin therapy reduces heart attack and stroke risk by 25% to 35% in people who need it. That’s huge. But if you stop taking it because of muscle pain, you’re trading short-term discomfort for long-term danger. About 1 in 5 cardiovascular events are linked to people not taking their meds as prescribed. The myth that vitamin D fixes statin intolerance might feel comforting. It gives patients and doctors a simple answer. But science doesn’t reward comfort-it rewards truth. And the truth is: vitamin D doesn’t solve statin intolerance. That doesn’t mean we’ve run out of options. We just need to look elsewhere. Maybe it’s timing your dose. Maybe it’s switching to a less muscle-reactive statin. Maybe it’s adding coenzyme Q10, though evidence there is also weak. The point is: don’t waste time on a fix that doesn’t work. Focus on what does.What to Do Next
If you’re on a statin and experiencing muscle pain:- Don’t stop the medication without talking to your doctor.
- Get your vitamin D checked if you’re at risk for deficiency (limited sun exposure, darker skin, older age, or obesity).
- If your level is low (<20 ng/mL), supplement to reach 30-50 ng/mL for general health-but don’t expect it to fix your statin side effects.
- Ask about trying a different statin. Pravastatin and rosuvastatin are often better tolerated.
- Consider non-statin options if side effects persist.
Final Thoughts
The idea that vitamin D could rescue people from statin intolerance was hopeful. It was simple. It felt right. But hope isn’t evidence. And now we have the best evidence we’ve ever had: vitamin D doesn’t help. Not in a meaningful way. Not for the majority of people. That’s not a failure. It’s progress. We’re learning what doesn’t work so we can focus on what does. For people struggling with statin side effects, the real solution isn’t a vitamin pill-it’s a conversation with a doctor who understands the options, the risks, and the real path to keeping your heart healthy.Can low vitamin D cause muscle pain from statins?
Low vitamin D can cause muscle weakness and pain on its own, which may make statin-related muscle symptoms feel worse. But correcting low vitamin D doesn’t reliably reduce statin-induced muscle pain, according to the largest and most rigorous study to date. The pain you feel on statins is likely caused by the statin itself-not your vitamin D level.
Should I take vitamin D supplements if I’m on a statin?
Only if your blood test shows you’re deficient. Vitamin D is important for bones, immunity, and overall muscle health. But taking it won’t make your statin easier to tolerate. Don’t take it hoping to solve muscle pain-take it because your body needs it.
Which statin is least likely to cause muscle pain?
Pravastatin and rosuvastatin are generally better tolerated than others like simvastatin or atorvastatin, especially in people with a history of muscle side effects. They’re less likely to build up in muscle tissue and have fewer interactions with other drugs. Your doctor can help you choose based on your cholesterol goals and medical history.
Is it safe to stop my statin if my muscles hurt?
No. Stopping statins without medical advice increases your risk of heart attack and stroke. Muscle pain is common, but it’s rarely dangerous. Talk to your doctor first. They can check your muscle enzymes, adjust your dose, switch your statin, or explore non-statin options. Don’t quit cold turkey.
Does vitamin D help with statin intolerance in people with severe deficiency?
Some small studies suggested yes, especially for people with levels below 20 ng/mL. But the largest, best-designed trial found no benefit-even in people with severe deficiency. The earlier positive results were likely due to other factors like improved lifestyle or placebo effects. Don’t rely on vitamin D as a solution for statin intolerance.

Marcia Facundo
This is such a relief to read. I’ve been taking vitamin D for a year thinking it was gonna let me stay on my statin, and I just kept feeling like a failure when it didn’t work. Turns out I wasn’t broken-just misled. Thanks for the clarity.
Ajay Kumar
Let me tell you something the medical industrial complex doesn’t want you to know. The 2022 JAMA study? Funded by Big Pharma. They’ve been pushing statins for decades and needed a way to keep people on them without admitting the drugs are inherently toxic. Vitamin D is a natural, cheap, non-patentable solution-so of course they spent millions to bury it. The real data? It’s buried in small clinics overseas where doctors still use it daily. You think they’d let a 2,000 IU supplement disrupt a $20 billion market? Please. The placebo group in that study probably got sugar pills laced with anti-inflammatory additives to skew results. Wake up.
Joseph Kiser
Look. I get why this feels like a punch in the gut. We all want simple fixes. We want to believe that popping a vitamin can save us from big scary drugs. But science doesn’t care about what we want. It cares about what’s real. The 2022 trial wasn’t just big-it was *rigorous*. Randomized. Double-blind. NIH-backed. And it found NOTHING. Not a whisper of benefit. That’s not a flaw. That’s the gold standard. If vitamin D worked, it would’ve shown up. It didn’t. So now we stop pretending. We stop wasting time on myths. And we start talking about real solutions: lower doses, different statins, ezetimibe, PCSK9 inhibitors. This isn’t defeat. It’s clarity. And clarity? That’s the first step to real healing. 💪
Hazel Wolstenholme
One must interrogate the epistemological foundations of the so-called ‘gold standard’ RCT paradigm, particularly when applied to nutraceutical interventions in complex, multifactorial physiological systems. The reductionist framing of vitamin D as a binary ‘on/off’ switch for statin tolerance ignores the pleiotropic, hormetic, and circadian-modulated nature of vitamin D metabolism. Furthermore, the exclusion of serum 25(OH)D kinetics, parathyroid hormone feedback loops, and genetic polymorphisms in GC and CYP2R1 renders the trial’s conclusions superficial at best. The 31% muscle pain incidence? Likely confounded by statin-induced coenzyme Q10 depletion, mitochondrial dysfunction, and myocyte membrane instability-all of which vitamin D may modulate indirectly. To dismiss it outright is not scientific rigor-it is scientism masquerading as evidence.
Mike Laska
I had to quit my statin after three weeks-cramps so bad I couldn’t walk to the fridge. I started taking 5,000 IU of D3 and guess what? I was back on the statin in two weeks. No pain. Zero. My doctor said it was placebo. I said, ‘Then why did my legs stop screaming?’ I’m not buying this ‘no effect’ nonsense. Someone’s lying. Either the study’s flawed… or my legs are haunted.
Alexa Apeli
Thank you for sharing this evidence-based perspective with such clarity and compassion. 🙏 It’s so important to separate hope from science-especially when our health is on the line. Let’s continue to advocate for personalized, thoughtful care, and always prioritize patient safety over convenient myths. You’ve done a wonderful service here. 💙
Eileen Choudhury
So many of us in India are low on vitamin D-sunscreen, dark skin, indoor jobs, pollution. I’ve seen people here get back on statins after D supplements and feel like new people. But I also know doctors here don’t always check levels. Maybe the problem isn’t vitamin D… it’s that the study was done in the US, where people are way more sedentary and have different diets. Maybe in places like mine, where people still walk to markets and eat turmeric with ghee, vitamin D matters more? Science should be global, not just American.
Zachary Sargent
They spent millions to prove vitamin D doesn’t help statins? Bro. They should’ve spent that on figuring out why statins wreck muscles in the first place. Instead we get this ‘you’re wrong for feeling pain’ vibe. I’ve been on three statins. All of them turned me into a walking zombie with cramps. My doctor said ‘take D.’ I did. Nothing. Now I’m off them. My heart’s fine. My legs are free. And I’m not gonna apologize for listening to my body.
Melissa Kummer
While the findings of the 2022 randomized controlled trial are indeed compelling, it is imperative to recognize that individual biological variability remains a critical factor in clinical practice. Although population-level data indicate no statistically significant benefit, anecdotal evidence from patients who experience resolution of myalgia following vitamin D repletion suggests that subphenotypes may exist. Further stratified analyses-by genetic markers such as VDR polymorphisms, baseline vitamin D status, and statin pharmacokinetics-are warranted. Until such research is conducted, clinicians should maintain a nuanced, patient-centered approach, balancing population evidence with individual clinical response. 🌿
andrea navio quiros
the study was good but what about people who actually feel better on d? i know people who couldnt walk then took d and now they can jog. maybe its not for everyone but its not nothing either. science is messy. real life is messier. if it helps someone dont take it away. just say maybe it works for some. not everyone is a statistic
Pradeep Kumar
I’m from Delhi and my dad’s on a statin. He was in pain, we checked his D-was at 12. Gave him 2000 IU daily. After 6 weeks, he said his legs felt lighter. He’s been on it for a year now. No pain. I know the big study says no effect. But my dad’s not a study. He’s my dad. Maybe it’s not magic. But maybe it’s enough. Let’s not throw out what helps real people just because the numbers say ‘no.’ 🙏
Andy Ruff
Let me be clear: if you’re still taking vitamin D thinking it’ll save you from statin side effects, you’re not just wasting money-you’re delaying real solutions. This isn’t ‘natural healing.’ It’s self-deception. Statins save lives. If you can’t tolerate them, it’s your body’s signal to find another option-not to chase vitamin myths. The placebo effect is powerful, but it’s not medicine. Stop fooling yourself. Your heart doesn’t care how you feel about supplements. It only cares if you’re alive next year.
Matthew Kwiecinski
The 2022 JAMA study had a flaw. They used 2,000 IU daily. That’s not enough for severe deficiency. Most people who respond to D need 5,000–10,000 IU to normalize levels. The study didn’t even stratify by baseline vitamin D. You can’t fix a deficiency with a toddler dose and expect results. This study didn’t disprove vitamin D-it proved that giving weak doses to everyone doesn’t work. Duh. What a waste of NIH money.
Justin Vaughan
Here’s the real takeaway: vitamin D doesn’t fix statin intolerance-but it doesn’t hurt either. If you’re low, take it. It’s cheap, safe, and good for your bones. But don’t bank on it to let you stay on a statin that’s wrecking your legs. Talk to your doc about alternatives. Lower dose. Different statin. Ezetimibe. Maybe even a non-statin approach. The goal isn’t to find a magic vitamin. It’s to keep your heart safe without turning your body into a cramp factory. You’ve got options. Don’t settle for myths.