High Blood Pressure Medication: Types, Interactions, and What You Need to Know
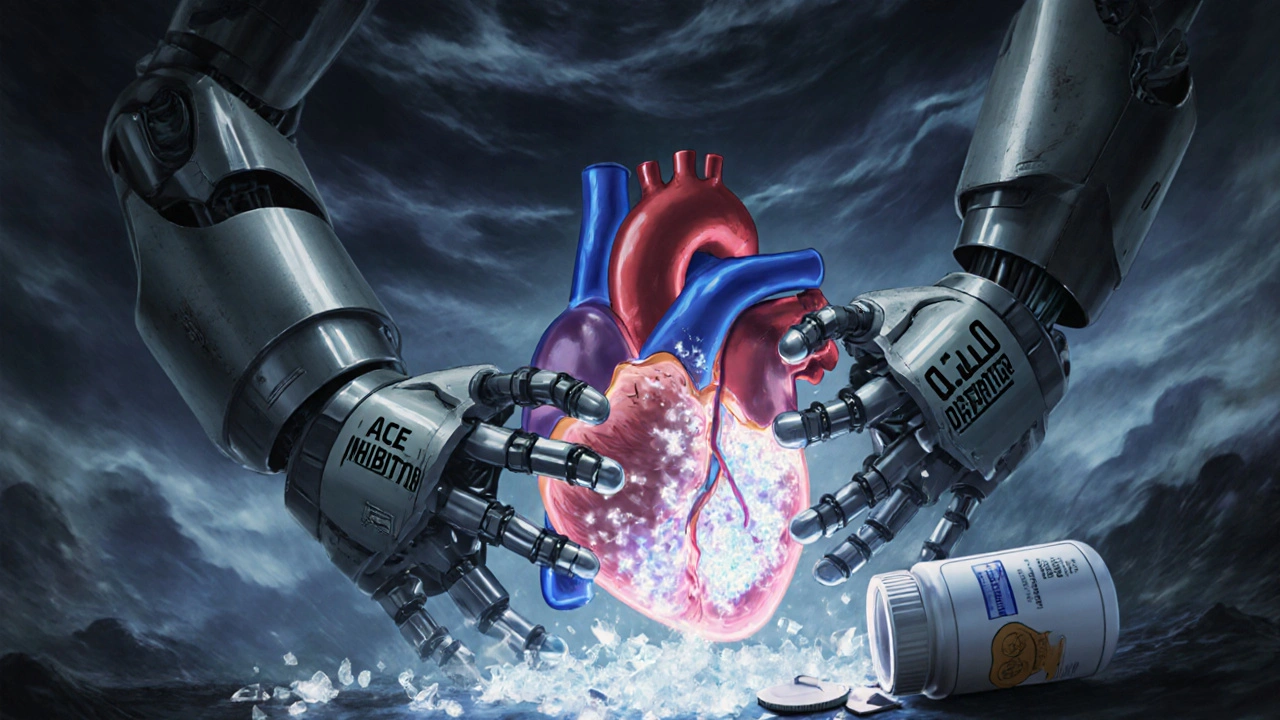
When you’re managing high blood pressure medication, drugs prescribed to lower elevated blood pressure and reduce risk of heart attack or stroke. Also known as antihypertensives, these medications are among the most commonly prescribed in the U.S.—and for good reason. Uncontrolled high blood pressure silently damages your arteries, heart, and kidneys over time. But taking the right one, at the right time, and knowing how it interacts with other drugs can make all the difference.
Not all high blood pressure medication, drugs prescribed to lower elevated blood pressure and reduce risk of heart attack or stroke. Also known as antihypertensives, these medications are among the most commonly prescribed in the U.S.—and for good reason. Uncontrolled high blood pressure silently damages your arteries, heart, and kidneys over time. But taking the right one, at the right time, and knowing how it interacts with other drugs can make all the difference.
Not all antihypertensives, drugs prescribed to lower elevated blood pressure and reduce risk of heart attack or stroke. Also known as high blood pressure medication, these medications are among the most commonly prescribed in the U.S.—and for good reason. Uncontrolled high blood pressure silently damages your arteries, heart, and kidneys over time. But taking the right one, at the right time, and knowing how it interacts with other drugs can make all the difference.
Not all medication interactions, when one drug changes how another works in your body, sometimes dangerously. Also known as drug interactions, these can turn a safe treatment into a risk—like mixing a blood pressure pill with an NSAID and suddenly seeing your pressure spike, or combining diuretics with lithium and risking kidney toxicity. These aren’t rare mistakes. They happen every day because patients don’t know what to ask.
And it’s not just about what’s in the bottle. Your diet, supplements, even over-the-counter cold meds can interfere. Fiber supplements like Metamucil can slow down how fast your blood pressure drug gets absorbed. Vitamin D doesn’t fix statin muscle pain, and neither does it help your blood pressure meds work better. Some people think switching to a generic version means the same effect—but authorized generics are exact copies, while regular generics can vary slightly in how they’re absorbed. That tiny difference can matter if you’re sensitive.
What You’ll Find in This Collection
Here, you’ll see real posts from people who’ve been there: how to track your provider’s advice so you don’t forget a warning, how to read labels so you avoid doubling up on active ingredients like ibuprofen or acetaminophen, and how to spot dangerous combos—like antidepressants with blood pressure drugs that can trigger serotonin syndrome. You’ll learn why some meds are avoided now (like Chloromycetin), how IVIG therapy can affect immune-related hypertension, and how heparin might quietly influence your mood. There’s no theory without practice here. Every post answers a question someone actually asked after a bad experience, a confusing label, or a scary side effect.
You won’t find vague advice like "eat less salt" or "exercise more." You’ll find specifics: when to take your pill in relation to your fiber supplement, how to recognize if your new generic looks different because it’s a problem, and which FDA alerts you should actually sign up for. This isn’t about guessing. It’s about knowing exactly what’s in your medicine cabinet—and why it matters.
Salt and Blood Pressure Medications: How Sodium Lowers the Effectiveness of Your Prescriptions
Cutting salt can make your blood pressure meds work better - sometimes as well as adding another pill. Learn how sodium affects your treatment, which foods to avoid, and how to reduce intake safely.