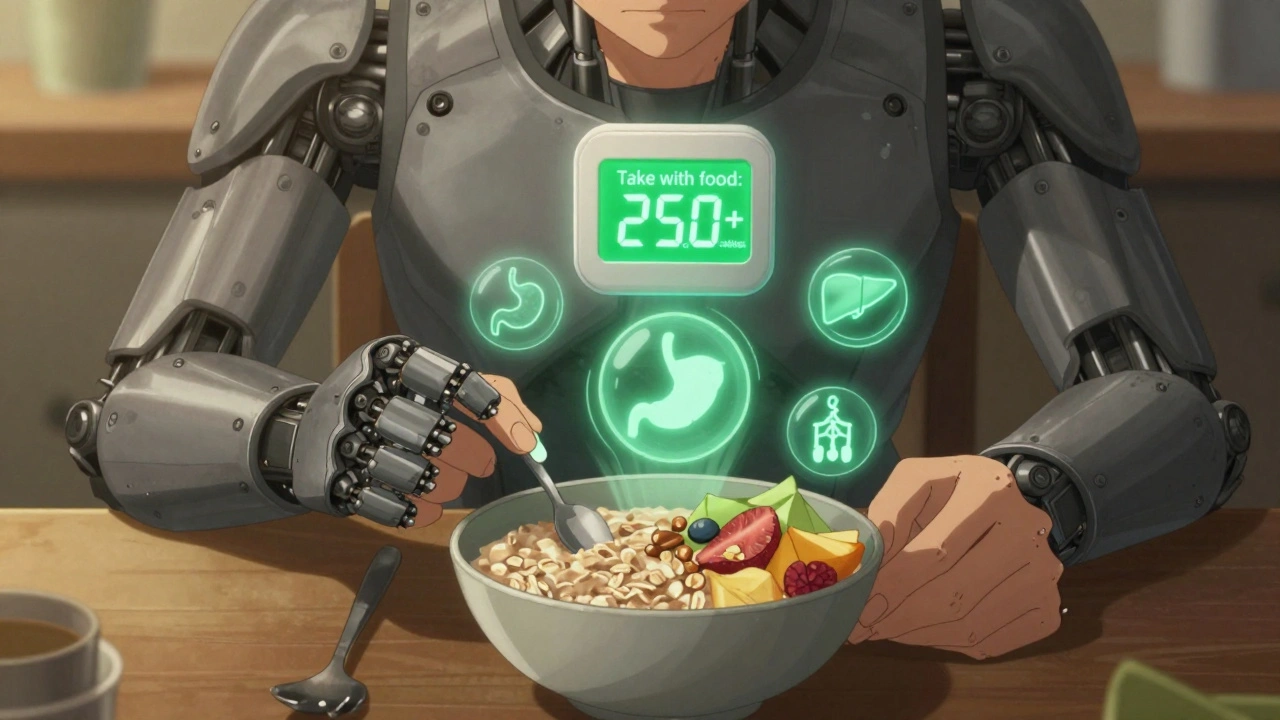
Medication with Food: How Eating Changes What Your Pills Do
When you take a medication with food, the presence of food in your stomach can change how quickly or completely your body absorbs the drug. Also known as drug-food interactions, this isn’t just a footnote—it’s a make-or-break factor for whether your medicine works at all. Take a pill on an empty stomach and it might zip through your system too fast, causing side effects. Take it with a big meal and it could barely get absorbed, leaving you with no benefit. It’s not magic. It’s chemistry.
Absorption, how your body pulls medicine into your bloodstream depends heavily on what’s in your gut. Some drugs, like certain antibiotics or antifungals, need fat to dissolve properly—so taking them with a glass of milk or a peanut butter sandwich boosts their effect. Others, like thyroid meds or some antibiotics, are blocked by calcium, iron, or even fiber. That’s why your pharmacist tells you to wait two hours before or after eating. Medication timing, when you take your pills relative to meals isn’t arbitrary—it’s science-backed advice to avoid wasted doses or dangerous spikes.
Not all interactions are obvious. Blood pressure meds like lisinopril can cause dizziness if taken with a high-salt meal. Cholesterol drugs like atorvastatin absorb better with food, but grapefruit juice? That’s a no-go—it can turn a safe dose into a toxic one. Even something as simple as a glass of orange juice can mess with certain antibiotics or heart meds. And don’t assume ‘natural’ means safe. Fiber supplements like Metamucil can trap pills and stop them from working unless you space them out by hours. These aren’t edge cases—they’re daily realities for millions.
What you eat doesn’t just affect absorption. It can change how your liver breaks down drugs, how long they stay in your body, and whether they build up to dangerous levels. That’s why mixing alcohol with sleep aids or painkillers is so risky. Your body’s already working overtime processing the alcohol, and adding medication can overload it. The same logic applies to high-fat meals and certain antidepressants or antipsychotics. One study found that taking the diabetes drug metformin with food cuts nausea by half—without reducing its effect. That’s a win.
There’s no one-size-fits-all rule. Some pills need food to protect your stomach. Others need an empty one to hit the bloodstream fast. The difference between a safe, effective dose and a useless or harmful one often comes down to whether you ate an apple or a burger 30 minutes before. That’s why reading the label isn’t enough—you need to know why the instructions exist. Your pharmacist isn’t just handing you a bottle. They’re giving you a map to make your medicine work.
Below, you’ll find real, practical guides on how food affects everything from blood pressure pills to antidepressants, sleep aids to diabetes meds. No fluff. No theory. Just what you need to know to take your meds right—and avoid the hidden risks most people never hear about.
Taking Medication with Food: When and Why It Reduces Side Effects
Taking medication with food can reduce side effects, boost effectiveness, or cause dangerous interactions. Learn which drugs need food, which must be taken empty, and how grapefruit, calcium, and even coffee can change how your medicine works.