Take Medicine With Food: What You Need to Know About Timing and Safety
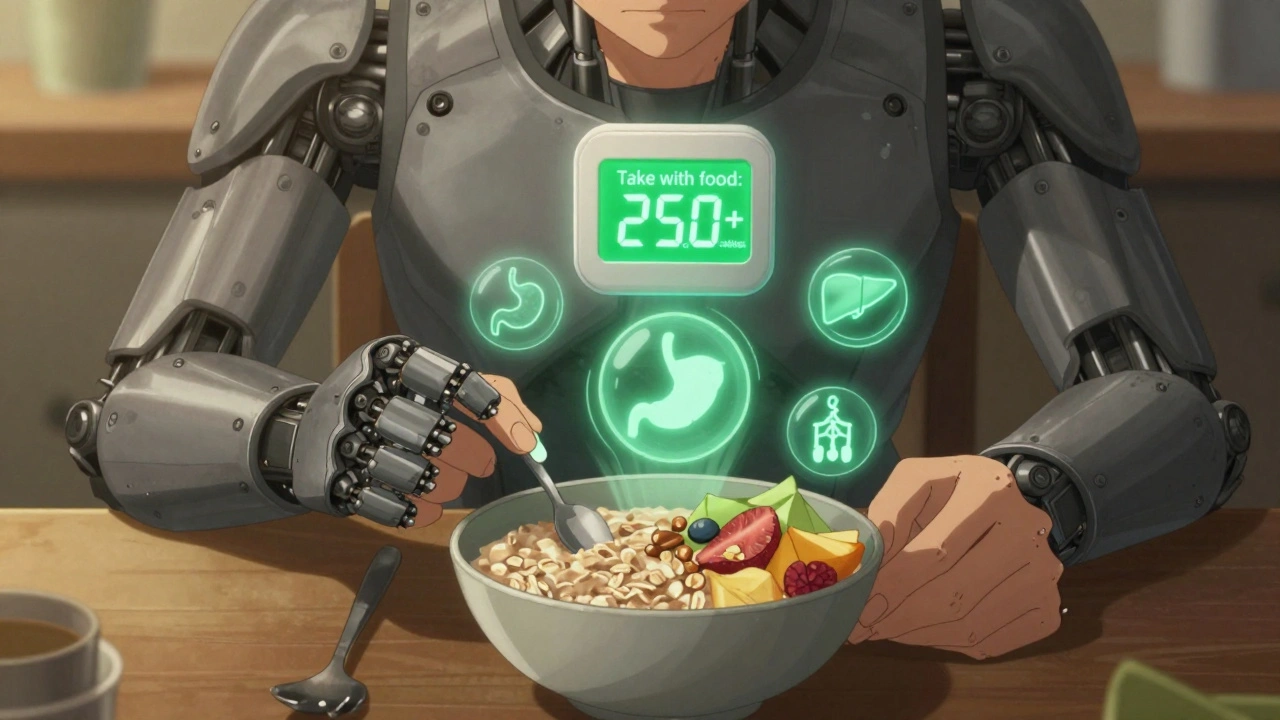
When you take medicine with food, the practice of consuming medications alongside or shortly after eating to affect how the body absorbs or reacts to them. Also known as taking drugs with meals, it’s not just a suggestion—it can mean the difference between a drug working properly or causing harm. Some pills work better when your stomach is full. Others become dangerous if you eat even a bite. It’s not about preference—it’s about chemistry, biology, and your body’s real-time response.
Why does this matter? Because food-drug interactions, how what you eat changes how your body handles medication are silent, common, and often ignored. For example, taking certain antibiotics like tetracycline with dairy can block absorption, leaving the infection untreated. On the flip side, drugs like ibuprofen or naproxen can wreck your stomach lining if taken on an empty stomach—food acts like a shield. Even something as simple as grapefruit juice can interfere with cholesterol or blood pressure meds, making them too strong or too weak. These aren’t rare edge cases. They happen daily, and pharmacists see the fallout.
Then there’s stomach irritation, the discomfort or damage caused by medications that are harsh on the digestive tract. Many painkillers, steroids, and even some antidepressants are designed to be taken with food—not because they’re better absorbed, but because they’re too harsh otherwise. Skipping food might save you a minute, but it could cost you an ER visit. And don’t assume all meds are the same. Some need a full meal to trigger the right absorption window. Others need an empty stomach so nothing slows them down. The label says "take with food," but it doesn’t say what kind of food, how much, or when. That’s where people get confused.
It’s not just about pills. Think about your daily routine. Do you take your thyroid med with coffee? Your blood pressure pill with a bagel? Your diabetes drug right after breakfast? Each of those choices has consequences. Some drugs need a consistent routine—same time, same conditions—so your body learns what to expect. If you take one with food today and on an empty stomach tomorrow, your levels swing. That’s not just inconvenient—it’s risky.
And here’s the thing: you don’t have to guess. The information is out there. Pharmacists know which drugs need food, which avoid it, and which are fine either way. But you have to ask. You have to check. You have to pay attention to the little details that most people overlook. Because when it comes to your health, timing isn’t just about convenience—it’s about control, safety, and effectiveness.
Below, you’ll find real, practical posts that break down exactly how food affects your meds—from how salt ruins blood pressure drugs to why fiber supplements can block your other pills. These aren’t theory pieces. They’re based on what patients actually experience, what pharmacists see every day, and what the science says. Whether you’re managing diabetes, dealing with side effects, or just trying not to mess up your routine, the answers are here.
Taking Medication with Food: When and Why It Reduces Side Effects
Taking medication with food can reduce side effects, boost effectiveness, or cause dangerous interactions. Learn which drugs need food, which must be taken empty, and how grapefruit, calcium, and even coffee can change how your medicine works.