Diabetes – What You Need to Know
When talking about diabetes, a chronic condition where the body cannot properly regulate blood sugar levels. Also known as high blood glucose, it affects millions worldwide and touches every aspect of health.
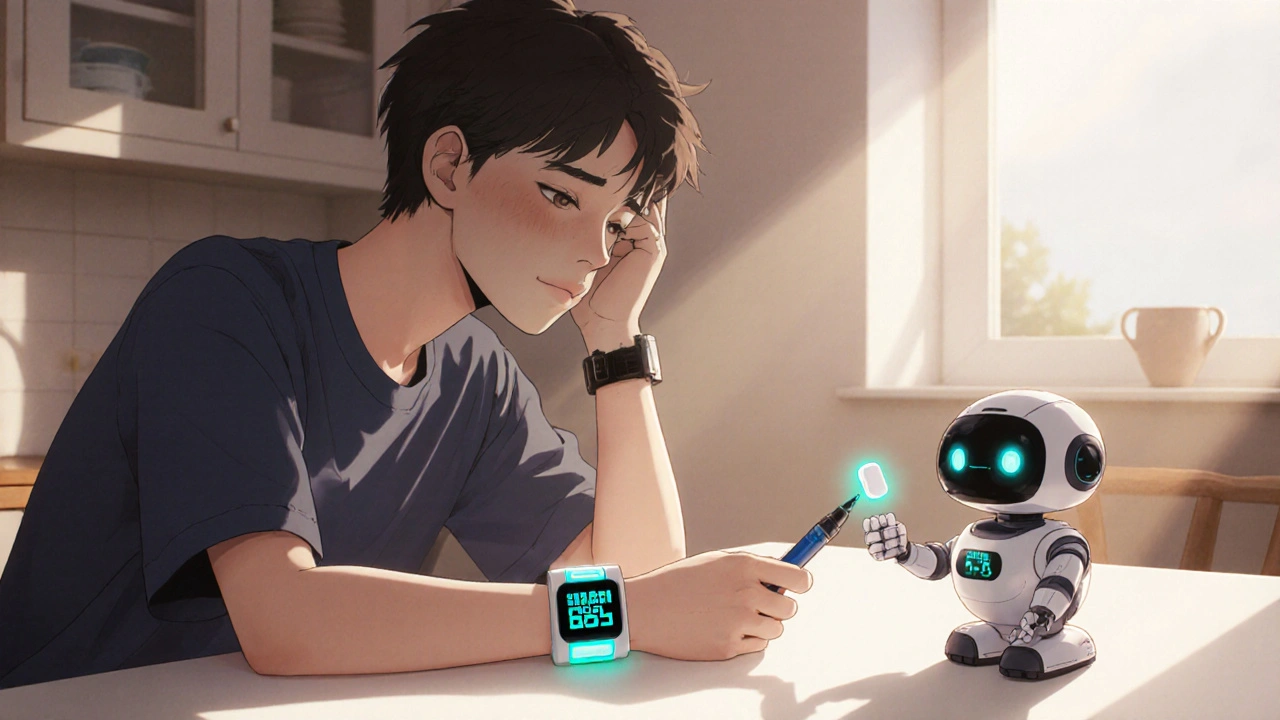
Living with diabetes means keeping a close eye on blood glucose monitoring, the process of measuring sugar levels in real time using meters or continuous sensors. This routine is the first line of defense because accurate numbers let you adjust food, activity, and medication before problems arise.
Most patients rely on insulin therapy, a hormone replacement that moves glucose from the bloodstream into cells. Whether you use rapid‑acting pens for meals or long‑acting injections for baseline control, insulin works hand‑in‑hand with diet and exercise to keep numbers steady.
Oral Medications and Their Role
When insulin isn’t enough or isn’t needed right away, doctors often prescribe oral hypoglycemic agents, pills that improve insulin sensitivity, reduce liver glucose production, or increase pancreatic release. Drugs like metformin, sulfonylureas, and SGLT2 inhibitors each target a different metabolic pathway, giving you a toolbox that can be customized to your lifestyle.
Diabetes doesn’t exist in isolation; it frequently overlaps with cardiovascular disease. High blood sugar speeds up plaque buildup, raises blood pressure, and harms blood vessels, which is why many of the posts on our site discuss beta‑blockers, antihypertensives, and cholesterol‑lowering meds. Knowing how these drugs interact helps you avoid side‑effects and plan a cohesive treatment plan.
Complications such as diabetic neuropathy, nerve damage that causes tingling, pain, or loss of sensation in the feet and hands, are common when blood sugar stays high for too long. Early detection through foot exams and regular nerve testing can stop the progression before it impacts daily life.
Beyond medication, diet and activity are the other pillars of control. Low‑glycemic carbs, balanced protein, and regular movement improve insulin response and lower the need for higher drug doses. Even small changes—like swapping sugary drinks for water or taking a brisk 30‑minute walk after meals—can shift numbers in a positive direction.
All of these pieces—monitoring, insulin, pills, heart health, and lifestyle—connect to form a comprehensive diabetes management strategy. Below you’ll find articles that break down each component, compare popular drugs, and offer practical tips you can apply right now. Dive in to deepen your understanding and take charge of your health.
Insulin Therapy Side Effects: Managing Hypoglycemia & Weight Gain
Learn how insulin therapy can cause hypoglycemia and weight gain, why it happens, and the latest tools and strategies to manage these side effects safely.