Generic Substitution: What It Is, Why It Matters, and How It Affects Your Meds
When your pharmacist hands you a pill that looks different from what you’re used to, that’s generic substitution, the practice of swapping a brand-name drug for a chemically identical generic version. Also known as generic dispensing, it’s a routine part of modern pharmacy—and it’s saving the U.S. healthcare system billions every year. But just because the active ingredient is the same doesn’t mean the experience is. Many patients stop taking their meds because the pill looks different, the packaging changed, or they were never told why the switch happened. That’s where confusion turns into risk.
Generic medications, are approved by the FDA to work the same as brand-name drugs in dosage, strength, and how they’re absorbed. Also known as therapeutic equivalents, they’re not cheaper because they’re weaker—they’re cheaper because they don’t carry the cost of marketing, research, or patents. But here’s the catch: not all generics are created equal in the eyes of patients or even doctors. Some prescribers still believe generics are less effective, even though studies show no difference in outcomes for most conditions. Meanwhile, patients worry about inactive ingredients—like dyes or fillers—that might cause reactions, especially if they have allergies or sensitivities. That’s why generic drug confusion, a common problem where patients mistake a generic for a different drug or think it’s inferior. Also known as medication appearance anxiety, it leads to missed doses, ER visits, and unnecessary fear.
And it’s not just about pills. Prescribing generics, is a skill that requires clear communication, trust, and education. Also known as generic prescribing, it’s more than checking a box on an e-prescription system. It’s explaining to a diabetic why their metformin now looks blue instead of white, or telling a patient with depression that their new generic sertraline has the same active ingredient as Zoloft. When providers skip that step, patients feel left in the dark. And when pharmacies switch without warning, trust erodes. That’s why the best outcomes happen when doctors, pharmacists, and patients all understand what generic substitution really means—and when it doesn’t.
You’ll find real stories here about people who stopped taking their meds after a switch, doctors who changed their minds after seeing the data, and pharmacists who started handing out simple color-coded guides to reduce confusion. You’ll also see how generic drug equivalence, isn’t just a regulatory term—it’s a daily reality for millions. Also known as bioequivalence, it’s the science behind why your generic blood pressure pill works just as well as the brand, even if the shape is different. These aren’t theoretical debates. They’re lived experiences—and they’re shaping how care is delivered today.
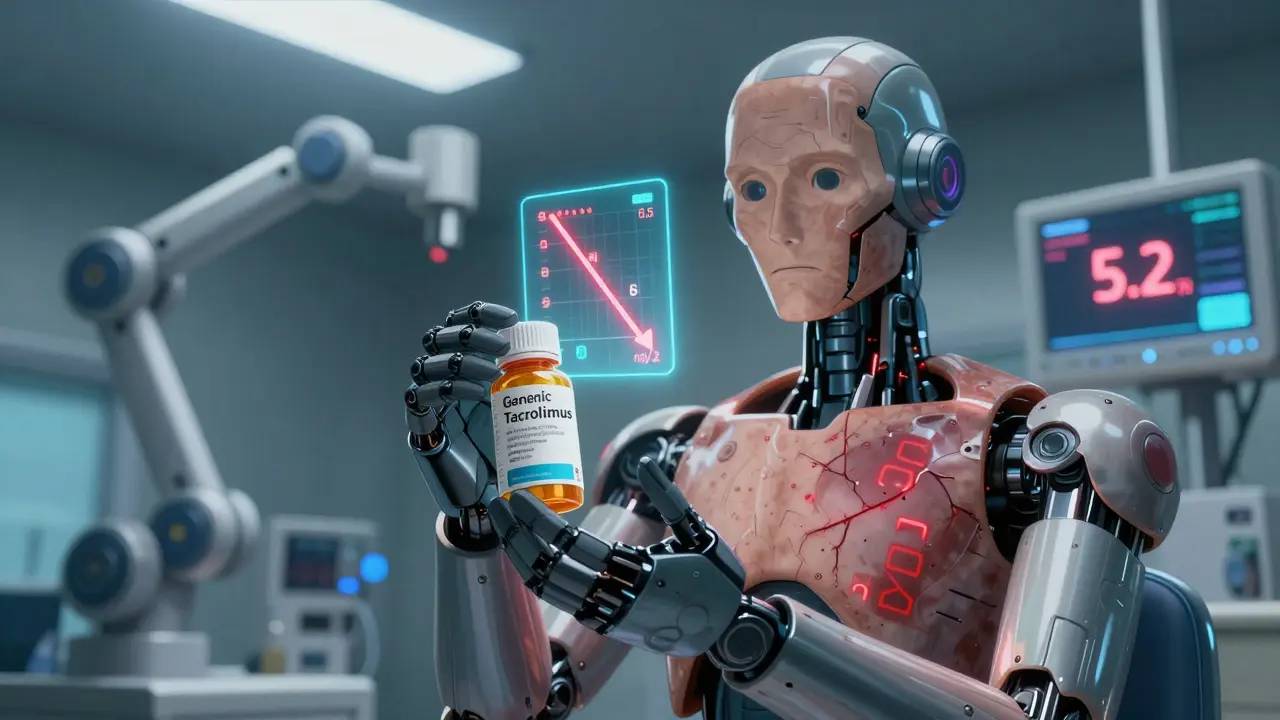
Cyclosporine and Tacrolimus Generics: What Transplant Patients Need to Know About Bioequivalence and Switching Risks
Generic cyclosporine and tacrolimus save money but carry serious risks for transplant patients due to narrow therapeutic ranges. Learn why switching brands can cause rejection or toxicity - and how to protect yourself.
Common Pharmacist Concerns About Generic Substitution: What They Really Think
Pharmacists support generic substitution to save patients money, but face resistance from patients who distrust cheaper drugs, doctors who don't promote them, and complex rules around high-risk medications. Learn why this common practice sparks real concerns behind the counter.