Medication Safety: Protect Yourself from Harmful Errors and Interactions
When you take a medication, medication safety, the practice of using drugs correctly to avoid harm, injury, or death. Also known as drug safety, it’s not just about following the label—it’s about understanding what happens when drugs mix, how to catch mistakes before they hurt you, and who to trust when something feels off. Too many people assume their doctor or pharmacist has already checked everything. But that’s not always true. A simple mix of over-the-counter painkillers and blood thinners can cause internal bleeding. A mood stabilizer like lithium can become toxic if you start taking a common NSAID like ibuprofen. These aren’t rare cases—they happen every day, often because no one asked the right questions.
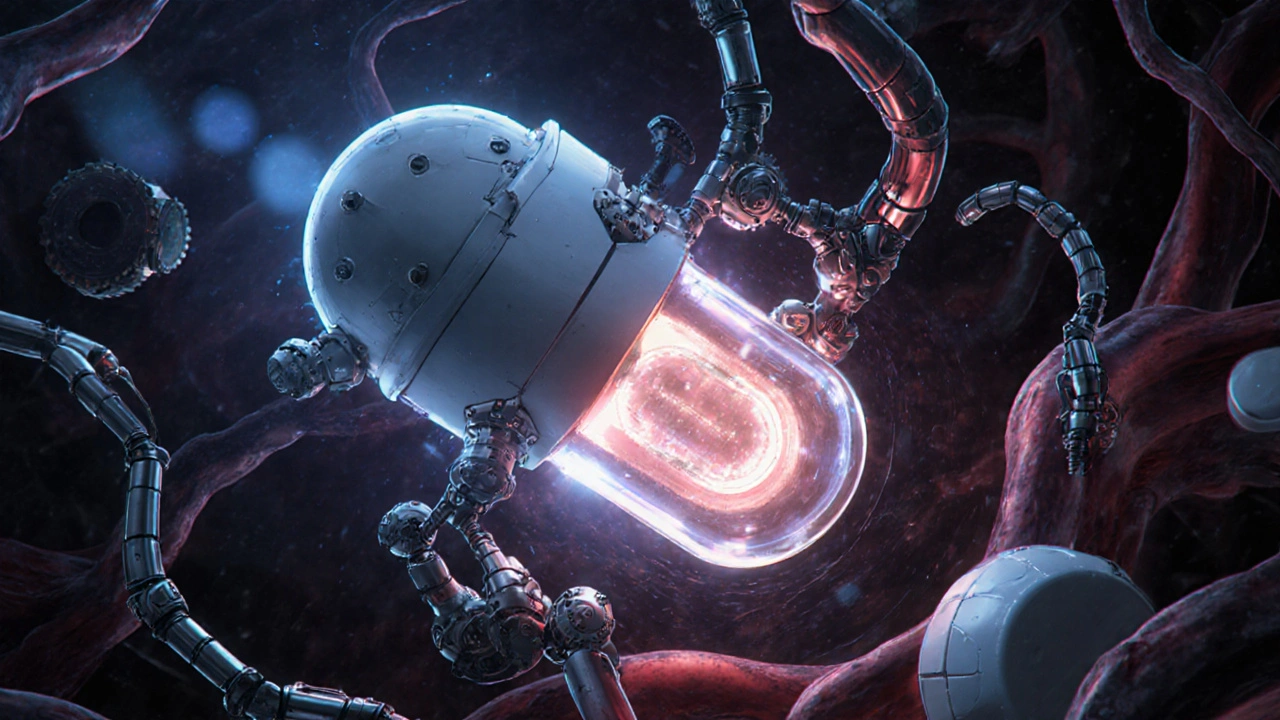
Drug interactions, harmful reactions that occur when two or more medications affect each other in the body are one of the biggest hidden dangers. The posts here cover real examples: SSRIs combined with MAOIs triggering serotonin syndrome, fiber supplements blocking lithium absorption, and even heparin affecting mood. These aren’t theoretical risks. They’re documented in clinical data and reported by patients who almost didn’t make it. Then there’s medication documentation, the practice of writing down what your provider tells you about dosing, side effects, and warnings. Most people don’t do it. They forget what was said after leaving the office. But writing down instructions—like when to take psyllium relative to metformin, or why you shouldn’t take vitamin D to fix statin muscle pain—can prevent hospital visits. And don’t forget FDA drug safety alerts, official warnings issued by the U.S. Food and Drug Administration about recalled or dangerous medications. These aren’t newsletters you can ignore. They’re urgent notices about drugs that might be contaminated, mislabeled, or linked to sudden deaths. Subscribing takes two minutes. It could save your life.
Medication safety isn’t just for seniors or people on ten pills a day. It matters if you’re a college student on atomoxetine, a new mom managing postpartum depression with antidepressants, or someone using garlic supplements alongside blood pressure meds. It matters if you’re using compounded meds with a beyond-use date you don’t understand, or if you’re taking an authorized generic and think it’s exactly the same as the brand name. The truth is, no one is immune to error. But you can protect yourself. Below, you’ll find clear, no-fluff guides on how to read OTC labels, track psychiatric drug risks, respond to side effects in kids, and know when to call 988 if you’re thinking about overdose. These aren’t theory pieces. They’re tools you can use today—because safety doesn’t wait for perfect timing. It starts with the next step you take.
OTC Drug Facts Labels: A Complete Guide to Reading and Using Them Safely
Learn how to read FDA-mandated OTC Drug Facts labels to avoid medication errors. Understand each section's purpose, common mistakes, and practical steps for safe use. Essential info for anyone using over-the-counter medicines.
How to Talk to Your Pharmacist About Using Expired Drugs Safely
Learn how to safely talk to your pharmacist about expired medications-when they’re risky, when they’re okay, and how to dispose of them properly. Avoid health dangers and save money with smart advice.
What to Do If You Receive the Wrong Medication from the Pharmacy: Immediate Steps and Legal Rights
If you receive the wrong medication from the pharmacy, act fast. Stop taking it, call your doctor, keep the pills as evidence, and report the error. You have legal rights-and your report could save someone else's life.
Questions to Ask Your Doctor Before Starting a New Medication
Know what to ask your doctor before starting a new medication to avoid dangerous side effects, interactions, and misunderstandings. Get the key questions backed by medical research and real patient experiences.
Comorbidities and Side Effects: How Existing Conditions Increase Drug Risk
Comorbidities like diabetes, heart disease, and kidney problems dramatically increase the risk of dangerous drug side effects. Learn how existing conditions alter drug metabolism, why polypharmacy is so risky, and what you can do to stay safe.
How to Read Prescription Labels to Avoid Dangerous Drug Interactions
Learn how to read your prescription label to spot dangerous drug interactions. Know what to look for, how to avoid mistakes, and why apps aren't enough. Your label holds life-saving info - here's how to use it.
EHR Integration: How Pharmacy-Provider Communication Is Transforming Prescription Safety
EHR integration connects doctors and pharmacies to share patient data in real time, cutting medication errors, reducing hospital readmissions, and improving adherence. Learn how it works, why adoption is slow, and what’s changing in 2025.
Active vs Inactive Drug Ingredients: Why the Difference Matters for Your Health
Active ingredients treat your condition, but inactive ingredients determine if your medicine works properly - and whether you have side effects. Learn why the difference matters for safety, effectiveness, and personal health.